Study Turns Up the "Volume" on Debate
Surgeons object to the assertion that busy refractive practices have the greatest risk
of malpractice claims.
BY JOSEPH HOFFMAN
Running a high-volume refractive surgical practice put surgeons at the greatest risk for a malpractice claim, according to a review of the database of the Ophthalmic Mutual Insurance Company (OMIC). Doing more than 300 cases per year was the greatest independent risk factor, and the risk was heightened if the practice advertised or co-managed patients referred by optometrists.
|
|
|
|
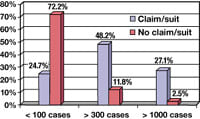
Comparison of annual refractive surgical volume and percentage of surgeons insured by OMIC who did or did not have malpractice claims or lawsuits filed against them. (Adapted from abstract of Abbott
RL. Medicolegal risk factors for ophthalmologists performing PRK and LASIK surgery. Paper presented at the annual meeting of the American Academy of Ophthalmology, Anaheim, Calif., November 15,
2003.) |
|
The retrospective cohort study of 100 consecutive OMIC claims and lawsuits related to LASIK and PRK from 1996 to 2002 was conducted by Richard L. Abbott, M.D., and coworkers at the University of California, San Francisco. The results, which were published in the November 2003 issue of the American Academy of Ophthalmology journal Ophthalmology, caused a stir in the audience when they were reported at the Academy's annual meeting during the Subspecialty Day on refractive surgery.
"The goal [of this study] was to provide statistically significant data for underwriting criteria and risk-management protocols, and proactively act to reduce the risk of claims and lawsuits against refractive surgeons," Dr. Abbott said. "Our goal also was to improve the quality of care for patients undergoing refractive surgery.... The good news is that the annual incidence of OMIC lawsuits peaked in 2002 and appears to be less in 2003 based on the data to October."
The data revealed some geographic trends. "The highest number of refractive surgeons... and the highest underwriting risk appear to be in the Pacific region," Dr. Abbott said. "The highest percentage of surgeons who applied for coverage for refractive surgery were in the Pacific region. Almost 50% [49.7%] of all ophthalmologists insured by OMIC in the Pacific region applied for refractive surgery privileges the highest in the country." Nationally, 33% of all ophthalmologists enrolled in OMIC perform refractive surgery.
It was no surprise that of the refractive surgery claims and lawsuits studied, 79.5% were related to LASIK procedures, 5.4% to PRK, and 15.1% to RK or AK. At the time of the review, 64% of the claims and suits were still pending.
"So literally, the jury is out on two-thirds of all these cases," Dr. Abbott observed. Still, the study found some statistically significant differences among different types of refractive surgical practices and how likely they were to be sued. "Our study results showed the chances for incurring a malpractice claim or suit for PRK or LASIK correlate significantly with a higher surgical volume and a history of a prior claim or suit," Dr. Abbott said. "There is increasing pressure to do higher-volume surgery because of the high overhead associated with the surgery. Many business models demand higher volume for financial success."
Average surgical volume in the group with malpractice claims or suits was 491 cases per year, and in the no-lawsuit group it was 162 cases per year. "This was highly significant," Dr. Abbott said.
The OMIC data were also broken down into three groups based on surgical volume: surgeons who performed fewer than 100 procedures per year, greater than 300 cases per year, and greater than 1,000 cases per year. A statistically significantly greater percentage of the higher-volume practices had claims filed against them. (See chart on page 147.)
The study showed additional risk factors related to advertising, comanagement, preoperative time spent with patients, and gender of surgeon, Dr. Abbott said. "The key element here was that these findings were all volume-dependent.... Unfortunately, unrealistic promises often led to unrealistic expectations, and less time with patients to less than desired outcomes, and the claim then was filed.
"So what do you do if you fall into this category?" Dr. Abbott asked. "You need to stop and think. You need to slow down. You need to pay attention to these risk factors... and act proactively to reduce the risks as you work with risk managers in your medical malpractice liability company."
This study once again raises the controversy over quality of care versus patient volume. The debate has been a longstanding one in ophthalmology, first in regard to cataract surgery and more recently with the growth of refractive surgery. A page on the UCSF department of ophthalmology Web site (ucsfeye.net/rabbottresearch.shtml) describes Dr. Abbott's work in developing practice guidelines for refractive surgery.
"I have had the opportunity to help create standards for improving the quality of eye care for our patients on a national and international level," the page says. "The elective nature and high patient expectations of refractive surgery present distinctive risk management challenges to ophthalmologists who perform this procedure. I have developed guidelines to assist practicing ophthalmologists in providing comprehensive and medically sound informed consent to their patients in an effective, ethical manner.... I have also developed specific guidelines and recommendations for advertising, considering its effects on the process of informed consent.... As the subspecialty of refractive surgery grows, I will continue to emphasize the importance of responsible, ethical behavior, which is paramount for patient care."
At Dr. Abbott's AAO lecture, some members of the audience could be heard expressing consternation at the volume/risk link. ("So is doing less surgery going to make me a better surgeon?" someone asked a colleague.) The chairman of the session echoed their sentiments in one of his follow-up questions. How can more-experienced high-volume surgeons have the lowest reported complication rates and also the greatest percentage of malpractice claims?
"Having a lot of experience and being a high-volume surgeon doesn't necessarily mean that you have a poor practice pattern," Dr. Abbott replied. "You can comanage, you can advertise, and you can do high-volume surgery. You just have to pay attention to the patient and have the right tools to do that."
Joe Hoffman has worked in medical communications since 1985 and is certified by the Board of Editors in the Life Sciences. He's the founder of Hoffman Healthcare Communications, LLC, which you can find on the Web at hoffmanhealthcare.com.
|
What About Incidence of Lawsuits Per Case? |
From his perspective as a busy surgeon in a thriving refractive surgical practice in Johnston, N.Y., John Kearney, M.D., saw the Abbott paper and AAO lecture as a purposely skewed view. "It was not a well-designed study," he said, "and it seems they had a foregone conclusion that they wanted to support." The obvious omission, Dr. Kearney said, was an analysis of the relative risk per case for high-volume vs. low-volume refractive surgeons. "I was there when the paper was delivered," Dr. Kearney said. "When [session moderator] Dr. Donnenfeld questioned him, Dr. Abbott admitted that he had never really looked at whether there was actually a lower incidence of lawsuits per case for high-volume surgeons. If you're going to do 1,000 refractive procedures vs. 1 procedure, of course your chances of being sued are higher, but your incidence of suits per case may be much lower. And this study didn't look at it from that point of view." Dr. Kearney also doubted the way that the study connected higher patient volume with less time spent with each patient. "Every surgeon has to spend time counseling their patients personally," he said. "Large practices can also have a surgical counselor to work with patients, and they have videos and printed materials. Those patients are probably better advised than patients who go to a low-volume practice that doesn't have the same resources. I always think of the sister at the first hospital I worked at who said she wouldn't want to be the last one of the 50 patients we operated on that day. I told her I'd rather be number 50 than number 1, and I still believe that today." Dr. Kearney voiced many of the frustrations expressed by other surgeons who looked to the study for guidance. "Well, you can't easily change from male to female," he joked, "and it's not practical to relocate from one part of the country to another. And if you've made a large capital investment in a surgery center you're not able to downsize to a small refractive surgical volume. The best way to proceed is to keep doing what you do well and pay attention to the details. Dot all the i's and cross all the t's." |
|
Were the Necessary Data There? |
When Richard L. Lindstrom, M.D., managing partner of Minnesota Eye Consultants (MEC) in Minneapolis, learned of the Abbott study, he reviewed the records of their high-volume, seven-surgeon anterior segment surgery practice. "During the time of the Abbott article [1996-2002], seven MEC surgeons performed 30,303 LASIK and PRK procedures," Dr. Lindstrom said. "All seven surgeons fit the paper's definition of a high-volume refractive surgeon, and all seven of our surgeons have significant cataract, corneal, and/or glaucoma surgical practices as well." Dr. Lindstrom said that there are six male and one female surgeons on staff at MEC, and the practice has always advertised and comanaged surgical patients with referring ophthalmologists and optometrists. The internal case review at MEC found 3 LASIK/PRK claims or lawsuits, for an incidence of approximately 1 per 10,000 refractive surgical procedures. All of those claims and lawsuits involved a single male surgeon who was also involved in legal action initiated by non-refractive surgical patients. One of those claims was from a comanaged patient and two were not. Dr. Lindstrom noted that this ratio matches the 1:2 proportion of comanaged/referred vs. internal surgical patients at MEC. Although there are lessons to be learned from the Abbott study, he said, some of the implicated "risk factors" may well be spurious. "I encourage all ophthalmologists to review the Abbott et al. article carefully and then to draft a risk management strategy for their individual practices," Dr. Lindstrom said. "A malpractice claim or lawsuit can have a devastating effect on surgeons, their practice, their partners and even their family and friends." Although the review of practice claims and lawsuit history could be construed to focus special attention on high-volume male surgeons, Dr. Lindstrom points out that the one female surgeon at MEC currently has the highest-volume refractive surgical practice and has not yet been subject to a claim or lawsuit. The MEC surgeons have decided not to reduce their surgical volume by limiting their marketing and referral/comanagement patterns. "We have, however, increased our effort to be certain that our marketing pieces are accurate, honest and formulated such that we would not be embarrassed to have them presented to a jury of our patients' peers," Dr. Lindstrom said. "Most importantly, we spend more preoperative time with our patients. As managing partner, I am encouraging this strongly in our practice. A strong doctor/patient relationship is the most powerful risk management tool available to any surgeon."
|
|
What Would Your Practice Records Tell You? |
Robert Lehmann, M.D., a busy anterior segment surgeon with offices in Nacogdoches and Grapevine, Texas, appreciated the study's focus on the need for risk management, but was dubious about some of the conclusions. "Data collection and the treatment of the data, as well as any existing bias, can have a great impact on conclusions for any given study," he said. "I don't see where this study actually matches the volume of cases to the occurrence of claims." Rather than establishing a link, the paper aligned data on surgical volume with data on the time spent with patients and the number of malpractice claims in what may or may not be a valid connection "A low-volume practice can do a good job of screening and counseling patients, and a conscientious high-volume practice can do a good job," Dr. Lehmann said. "But practices that do not take time or aren't well equipped to counsel patients can have a greater incidence of claims, regardless of how many procedures they do. Either way, it's really a question of the number of claims per patients treated in the practice, which is what this study did not seem to address." He agreed, however, that geography was correctly identified as a risk factor. "It is a fact that we are in a litigious society," Dr. Lehmann said, "and that LASIK is a leading target for claims. It has been documented that there are certain regions that are more suit-prone." He believes the Abbott study did not have all pertinent data, however, to interpret the connection between surgical volume, surgeon-patient interaction, and the risk of malpractice claims. "We have been doing a significant volume of laser vision correction cases since 1996," Dr. Lehmann said. During that time, just one claim was made against the practice, and that claim was dropped even before depositions were taken and with no settlement agreement. "If you keep abreast of the published studies and current standards, if you evaluate Orbscan data, corneal topography, pachymetry, pupil size, and wavefront data, and if you counsel patients regarding expectations and exclude those who are not suitable candidates for surgery, you will definitely limit your potential liability." In addition, keeping abreast of current technology is critically important. "I began the transition to the Intralase femtosecond laser technology for creation of the LASIK flap one year ago. This has reduced my stress more than any other single factor with regard to the surgery itself." |