LASEK
Gains Ground on LASIK
New techniques and post-op regimens make it
a competitive alternative.
BY MARGUERITE MCDONALD, M.D.
Dr. Massimo Camellin introduced LASEK in 1999 in an effort to overcome the limitations of surface ablation by PRK and also to eliminate potential complications from use of a microkeratome in LASIK. His original technique involved the use of alcohol to separate the corneal epithelium from the stroma and create an epithelial "sheet" that could then be repositioned over the ablated stroma.
The advantages of LASEK vs. PRK are that it can provide a postoperative shield of epithelium over the treated surface; it may prevent a wave of epithelial migration in the first 48 post-op hours; it prevents interaction between injured stromal tissue and factors released by corneal epithelial cells; and may have a lower incidence of haze than PRK.
Alcohol toxicity is the greatest potential drawback to classic LASEK. This toxicity is both dose- and time-dependent. In vitro cell survival has been shown to be reduced when concentration exceeds 25% or exposure period is longer than 35 seconds. The upper limit in which cells remain viable may be up to 45 seconds in 20% solution.
There is also some patient variability regarding adhesion of the epithelium to basement membrane and the effect of alcohol on the adhesion of epithelial cells. A solution of 20% alcohol applied for 20 seconds is reportedly sufficient to create an epithelial sheet, although Litwak et al. found that 20% alcohol needed a minimum exposure time of 40 seconds in Hispanic patients to loosen the epithelium.
Surgeons would like to eliminate the use of alcohol so that these variables will no longer be at issue. Several approaches are being explored. At our center, we are investigating gel-assisted epithelial separation. Drs. Rashid and Langerman are working on a hydrodissection method. Dr. Pallikaris is developing a technique he calls epi-LASEK, which uses a keratome with a dull-edged, flexible plastic separator designed to slide under the epithelium without applanation of the cornea.
|

|

|
|
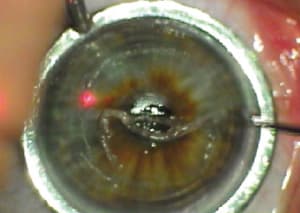
LASEK as described by Camellin begins with the creation of a corneal epithelial sheet by applying ethanol for 20 seconds. The sheet is "rolled up" using a spatula. Stromal ablation is then applied. After ablation, the epithelial sheet is repositioned over the treated area. |
||
A Better Match for Wavefront Ablation?
The interest in surface ablation has been increasing recently because early studies of customized ablation have shown that wavefront-guided surface ablation provides better results than wavefront-guided LASIK. This is because the creation of a LASIK flap produces unpredictable biomechanical changes in the cornea. This creates unpredictable changes in the wavefront status of the eye and unpredictable postoperative higher-order aberrations. Surface ablation eliminates the optical variables of the flap, and flap-free surgery certainly has its own appeal for patients and surgeons (no possibility of intraoperative flap complications, no postoperative diffuse lamellar keratitis, etc.).
|
|
|
|
Achieved versus intended correction of 31 eyes 1 month after CustomVue treatment with
LASEK. |
It is now possible to reduce postoperative pain and increase the rapidity of the return of vision enough to make surface ablation "competitive" with LASIK.
I performed a prospective, nonrandomized study of wavefront-corrected CustomVue LASEK in 31 myopic and myopic/astigmatic eyes using a classic alcohol-assisted technique. Three eyes were excluded from the study: one case each of mild amblyopia, trauma, and mental illness. LASEK was performed as an off-label indication with the Visx Star S4 laser, and I made no nomogram adjustments. Maximum follow-up was up to 6 months.
Our standard postoperative regimen of a bandage contact lens and topical anti-infective, steroid, artificial tears, and nonsteroidal anti-inflammatory drops was employed, except for the addition of "comfort drops" of dilute tetracaine (1:20 solution of 1% tetracaine). Patients find that using these drops for the first 3 days after surgery helps to minimize discomfort.
Mean preoperative MRSE in this group was -4.85D (range: -1.88 to 6.50), mean preoperative cylinder was +0.99D (range: 0 to +2.75), and mean preoperative BCVA was 20/20 (range: 20/15 to 20/30).
At 1 day postoperatively, mean UCVA was 20/40 (range: 20/16 to 20/63). At 6 to 7 days postop UCVA had improved to a mean of 20/25 (range: 20/16 to 20/50), which is certainly a good functional level of vision just a week after surgery. At the 1-month follow-up (n = 29), mean UCVA was 20/20+, with a range of 20/12.5 to 20/50. The mean MRSE was -0.07D (range: -1.25 to +0.63D), which is very close to plano. Predictability was also very good, with only a slight tendency toward undercorrection.
All 31 patients were able to drive without glasses by one day post-op because each had at least one eye that was 20/40 uncorrected. The quantity and quality of vision improved dramatically during the first week after the procedure and for at least 3 months thereafter.
Patients continued to improve through the 3-month follow-up (n=22). Mean UCVA was 20/20+ (range: 20/12.5 to 20/40), with a mean MRSE of -0.26D (-1.25 to +0.25D). The four eyes for which we have 6-month follow-up were all seeing 20/20 uncorrected, with a mean MRSE of -0.34D (range: -0.87 to +0.50D).
Next Puzzle: Corneal Wound Healing
With the new techniques and improved postoperative regimens, LASEK is now a competitive alternative to LASIK. Outcomes of wavefront-guided LASEK are actually better, even without a nomogram adjustment, and the procedure is safer because no flap is created. More advanced forms of surface ablation such as epi-LASIK may also allow us to unlock the secrets of corneal wound healing.
Dr. McDonald is a clinical professor of ophthalmology at Tulane University and the director of the Southern Vision Institute in New Orleans.
|
Why Epi-LASIK is Looking Good |
||||||
Now that interest in surface ablation is once again increasing with the introduction of wavefront-guided ablation, the new frontier seems to be an automated LASEK procedure performed without alcohol. Dr Ioannis Pallikaris has developed a new keratome to perform a procedure that he calls epi-LASIK. This instrument uses a flexible plastic separator with a dull edge. No applanation of the cornea is necessary, and the separator slides under the epithelium along the path of least resistance, leaving the basement membrane intact. The instrument is designed not to engage stroma. Studies performed in pig eyes verified that this keratome left a smooth surface. A recent report by Dr. Pallikaris on 34 myopic eyes of 17 patients treated with epi-LASIK stated that epithelial separation was achieved in 100% of cases. The post-op regimen included bandage contact lenses, anti-infectives, steroids, and nonsteroidal anti-inflammatories, but no "comfort drops" of dilute anesthetics. Only one of the 17 patients reported moderate post-op pain, and this was due to a tight bandage contact lens. One advantage of this instrument and technique may be that it cleaves the basement membrane underneath the laminas lucida and densa, at the level where it contacts Bowman's layer. Human histopathology studies have shown that epi-LASIK leaves the basal cells and their hemidesmosomes (which act as mechanical "fasteners") attached to the epithelium, which should improve the reattachment of the epithelium. Alcohol splits the basement membrane. Since the adherence of the basement membrane to the basal layer of the epithelium is significant for the viability of an epithelial sheet, we assume that the cleavage plane of the mechanical epi-LASIK separation may be superior.
|
||||||












