Controlling Glaucoma
With Early Potent Therapies
Preserving vision is a priority for patients with glaucoma. Read on to find out how you can use current research to make a difference.
By George Baerveldt, M.D., Irvine, Calif.
About 2.2 million Americans age 40 and older have primary open-angle glaucoma (POAG); some 87,800 Americans age 40 and older were blind from POAG in 2000.1
Mounting evidence indicates that reducing IOP is the best strategy for preventing and treating glaucoma -- and may even prevent vision loss.
Identifying Glaucoma
The American Academy of Ophthalmology (AAO) defines glaucoma as an optic neuropathy, characterized by progressive optic disc cupping and visual field loss. Although this disease is associated with retinal ganglion cell death, the major risk factor is increased IOP. Patients with IOPs higher than 30 mm Hg are more than 38 times more likely to have glaucoma than those with IOPs less than 15 mm Hg.2 In addition to IOP, other glaucoma risk factors include:
- Advanced age
- Ethnicity (higher prevalence among African-American and Hispanic people)
- Family history
- Possibly, diabetes mellitus and vascular dysfunction at the optic nerve.
Although elevated IOP may be the main risk factor for glaucoma, it isn't the definitive factor for diagnosing the disease. Up to 50% of patients with glaucoma have initial IOPs less than 21 mm Hg,2 and less than 10% of those with elevated IOPs have visual field loss from glaucoma.3,4
Diagnosing glaucoma depends on the ability to detect deterioration in the optic nerve, the retinal nerve fiber layer (RNFL) or the visual field. In addition to pachymetry, we need reliable imaging methods to follow our patients and to identify changes in the optic nerve and the RNFL.
The decision to lower IOP as a therapeutic priority is an example of evidence-based medicine. In particular, five recent studies reinforce the value of lowering IOP in preventing glaucoma progression.
Early Manifest Glaucoma Trial
In the Early Manifest Glaucoma Trial (EMGT), Heijl and colleagues5 compared the benefit of IOP-lowering therapy with watchful waiting for patients with early POAG. The study randomized 255 patients to argon laser trabeculoplasty (ALT) plus topical betaxolol or to no initial treatment.
Investigators followed patients at 3-month intervals for 4 to 9 years. They were able to analyze the IOP-lowering effects of these two modalities because of a large IOP gradient in the group treated with ALT and betaxolol. Their findings provided definitive evidence that lowering IOP prevents disease progression in glaucoma, including:
- Each 1 mm Hg decrease in IOP lowered the risk of glaucoma progression by 10%.
- Fewer treated patients had glaucoma progression (45%) compared with untreated patients (62%). (See "EMGT: Early Treatment Reduces and Delays Glaucoma Progression.")
- On average, when patients had disease progression, treated patients took 66 months to show progression of the disease, compared with 48 months for untreated patients.
- Even slight improvements in lowering IOP decreased and delayed the progression of early glaucoma. (See "EMGT: Fewer Treated Patients Have Glaucoma Progression.")
 |
 |
 |
 |
Collaborative Initial Glaucoma Treatment Study
The goal of the Collaborative Initial Glaucoma Treatment Study (CIGTS) was to test if medical therapy or filtration surgery is more beneficial for newly diagnosed POAG patients.
Lichter and colleagues6 prospectively randomized 607 patients to receive either medication or surgery and followed them for 5 years at 6-month intervals. The treating physicians set individualized target IOPs according to a formula that took into account baseline IOP and visual field loss. A 25% decrease from baseline was required for a patient with baseline IOP of 25 mm Hg and no field damage; if minor field damage (scored as 5) was present, the researcher set the target pressure 30% lower than baseline IOP.
Each treatment strategy lowered IOP and helped prevent visual field loss. IOP decreases were excellent with both approaches but were slightly better with surgery. (See "CIGTS: Medical Management vs. Surgery: Both Lower IOP.") Finally, both treatments reduced IOP by 38% to 46% and the risk of significant field loss at any visit to 10.7% to 13.5% over 5 years. (See "CIGTS: Medical Management vs. Surgery: Both Prevent Visual Field Loss.")
The lesson of CIGTS is that effective therapy to achieve individualized target IOP lowering can slow disease progression in newly diagnosed glaucoma patients.
Advanced Glaucoma Intervention Study
In the Advanced Glaucoma Intervention Study (AGIS),7 researchers compared the effectiveness of laser and incisional IOP-lowering surgery in glaucoma patients who had elevated IOPs despite medical therapy.
Investigators randomized a total of 789 eyes to initial ALT or trabeculectomy and followed the patients for 8 years after treatment. Retrospective analyses of IOP-lowering and glaucoma progression answered two important questions:
1. Does IOP during the first 1.5 postoperative years predict later visual field loss?
2. Are consistently low pressures associated with stable visual fields?
Researchers found that patients who had higher IOPs in the early years after surgery had greater visual field loss after 96 months' follow-up. What's more, patients whose mean IOPs were higher than 17.5 mm Hg had a significantly higher risk of glaucoma damage. (See "AGIS: Higher IOP Predicts More Visual Field Loss in Advanced Glaucoma.")
Patients whose IOPs were lower than 18 mm Hg at all visits had virtually no change in visual defect. However, the data showed that even small differences in patients' mean IOPs significantly affected visual field loss. (See "AGIS: Consistently Low IOP Reduces Vision Loss in Advanced Glaucoma.")
Results from the AGIS study demonstrate that the goal of initial treatment should be to consistently lower IOP below 18 mm Hg. Subsequent therapy should focus on getting IOP as low as possible to prevent further deterioration in advanced glaucoma. Patients with a mean IOP of 12.3 mm Hg didn't have disease progression, whereas those with a mean IOP of 14.7 mm Hg on average lost 1 visual field unit. Effective treatment to achieve very low pressures ensures the best results.
|
|

|

|
|
Ocular Hypertension Treatment Study
The Ocular Hypertension Treatment Study (OHTS)8 investigated the safety and efficacy of using topical medications to delay and prevent the onset of glaucoma. In addition, the investigators sought to determine which patient characteristics increased the risks of developing glaucoma.
Physicians randomized 1,636 patients to observation or topical glaucoma medication for 5 years. The goal of medication was to achieve a 20% IOP reduction and a target IOP lower than or equal to 24 mm Hg. Some 9.5% of untreated patients developed POAG, compared with 4.4% of patients who received treatment. (See "OHTS: IOP Lowering in OHT Reduces the Incidence of POAG.") Patients with thicker corneas and a smaller cup/disc (c/d) ratio were also less likely to develop POAG.
The major implication of the OHTS is that lowering IOP can prevent the development of glaucoma in OHT patients. This suggests that many OHT patients should be treated to reduce their IOP and that the benefits of treatment could outweigh the costs for patients at highest risk of glaucoma. Such patients include those with thinner central corneas, higher IOPs, larger c/d ratios or advanced age.
Interestingly, OHTS suggested that race, per se, doesn't influence disease progression. Rather, physicians found that participating African-Americans had thinner corneas and larger c/d ratios, which accounted for their increased incidence of glaucoma.
|
|
Compensating for Corneal Thickness |
|
When measuring IOP, you must always take the patient's central corneal thickness into account. Patients with thin corneas have deceptively low IOP readings; We have yet to reach a consensus on the best way to compensate for corneal thickness when measuring IOP. The following method is based on meta-analysis of trials with IOP and corneal thickness measurements:
|
Collaborative Normal-Tension Glaucoma Study
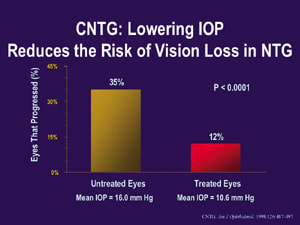
To determine if IOP-lowering treatment slows the progression of normal-tension glaucoma, the Collaborative Normal-Tension Glaucoma Study (CNTG)9 randomized 140 eyes to medical or surgical treatment (target was 30% below baseline) or no treatment. Investigators evaluated patients for threatened central fixation loss, proven history of progression or disc hemorrhage before randomizing them to either group. Treating physicians used multiple readings throughout the day to establish baseline IOPs.
Results showed that mean IOPs for untreated and treated eyes were within normal range (16 mm Hg and 10.6 mm Hg, respectively). However, treated eyes with lower IOPs showed less disease progression than untreated eyes: 12%, compared with 35% of untreated eyes. (See "CNTG: Lowering IOP Reduces the Risk of Vision Loss in NTG.") These results demonstrate that lowering IOP can slow disease progression in normal-tension glaucoma.
Clinical Applications
Compelling results of current research provide insight into the relationship between IOP and disease progression in glaucoma. We now face the challenge of using this knowledge to develop practical IOP-lowering strategies that can help us preserve our patients' sight.
Dr. Baerveldt is the Irving H. Leopold Professor and chair of the department of ophthalmology, University of California, Irvine.
References
1. Friedman DS, De Jong PT, Klein BE, et al. Glaucoma prevalence in the United States: Results of a meta-analysis. Presented at the American Glaucoma Society (AGS) Annual Meeting. March 69, 2003; San Francisco.
2. Sommer A, Tielsch JM, Katz J, et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans: The Baltimore Eye Study. Arch Ophthalmol. 1991;109:10901095.
3. Leibowitz HM, Krueger DE, Maunder LR, et al. The Framingham Eye Study monograph. Surv Ophthalmol. 1980;24(suppl):335610.
4. Bengtsson B. The prevalence of glaucoma. Br J Ophthalmol. 1981;65:4649.
5. Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: Results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120:12681279.
6. Lichter PR, Musch DC, Gillespie BW, et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108:19431953.
7. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130:429440.
8. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: A randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701713.
9. Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487497.









