Practice-Building with the
Array
Thanks in part to its effect on presbyopia, the multifocal IOL has done a lot for this practice.
BY TOM M. COFFMAN, M.D.
Traditional cataract surgery and LASIK have provided patients with spectacle independence for distance vision. However, most presbyopic patients still use spectacles for near vision, and today's cataract patients are eager to avoid this.
Since I began offering the Array Multifocal IOL in my practice, it's possible to give them what they want -- at least to a large extent. Clinical studies have demonstrated that patients implanted with the Array achieve both good distance and near visual acuity postoperatively, along with low levels of spectacle use. As a result, this lens not only allows you to offer an exceptional result to cataract patients, but provides a new refractive surgery option to offer to non-cataractous presbyopes.
Off and Running
Our own experience demonstrates the practice-building potential of the Array IOL. We began offering the Array as an option for patients who wanted spectacle independence in 1997. In January of 1998, we invested in 3 months of radio, TV and newspaper ads to make more people aware of the lens. As a result of that investment, our cataract surgery practice grew 30% within the first 4 months.
Since that time our cataract surgery practice has grown about 10% annually. This growth has been sustained mainly by word of mouth, with minimal marketing since the introductory period. In fact, patients often come to us for the Array (on their own) after another ophthalmologist tells them they need cataract surgery.
We don't charge extra to implant the lens in our cataract patients if we believe it's their best option, in part because it produces happier patients who generate more business.
Offering Refractive Lensectomy
We also include the Array IOL in our refractive options bundle along with LASIK, even though refractive lensectomy isn't an FDA approved indication for the Array. We market it as "Bifocal Reduction" surgery, with a 30-minute infomercial once or twice a month, and 30-second radio ads. We also use internal marketing.
Bifocal Reduction patients receive VIP treatment, including 1 year of follow-up care. Pre-op counseling is done by the surgeon, who explains the treatment to the patient and supplies brochures for the patient to take home.
In general, we charge about twice as much for refractive lensectomy as we charge for LASIK. However, patients are willing to spend the extra money. (Currently, this has the highest profit margin of any procedure we offer.)
As the general population becomes more familiar with this procedure, I believe it will become increasingly popular.
Ensuring Successful Outcomes
Over the years we've learned to maximize the likelihood of positive outcomes by following certain basic strategies:
Offer the procedure to the right patients. Patients of any age, prescription or personality can be successful with the Array IOL. However, the best candidates are generally:
- cataract patients with the potential to achieve a visual acuity of 20/30 or better, with no corneal abnormalities
- individuals who understand the range of vision the Array IOL can provide, and can accept that it may take several months to totally adapt to the new visual system
- hyperopes, because their vision has generally never been extremely precise, and because they've usually been spectacle-free until near the onset of presbyopia.
Candidates who may not be satisfied with the lens include patients who demand "perfect" vision without spectacles, and those whose livelihood depends on night driving.
Provide extra pre-op counseling. It's important to spend extra time counseling Array patients both pre- and postoperatively. Preoperatively, we want them to have realistic expectations:
- We explain that the Array IOL will likely provide them with decreased spectacle dependency and the ability to enjoy a range of vision, from near to far.
- We discuss the limitations of the treatment, such as the fact that there is no guarantee that the patient will be spectacle-free, and that the patient may need spectacles for reading fine print or night driving.
- We explain the possibility of experiencing glare or halos with the Array IOL. (This is less of an issue for hyperopes, who generally have already adjusted to seeing halos.)
- Finally, we explain to the patients that there will be an adjustment period of up to several months as their brain adapts to a "new" visual system.
At the end of the preoperative counseling session, we have the patient sign a short summary of what was explained in the session.
Maximize the accuracy of your biometry. This is critical to the success of the Array IOL.
- Technicians with experience performing preoperative biometry make a big difference.
- Use the best technology available. AMO recommends laser interferometry for accurate axial length measurements. (We're evaluating the IOLMaster in our practice, but we've been able to achieve excellent outcomes without it.)
Have the procedure performed by an experienced surgeon. The implantation procedure for the Array is the same as for the SI40NB silicone monofocal IOL; surgeons should implant the SI40NB IOL in 20 to 80 patients to become comfortable with the refractive results.
Today, we only hire ophthalmologists who already have experience implanting the Array, and we continually refine our techniques to improve our outcomes.
Manage astigmatism. We usually treat astigmatism of 1D or more during surgery using limbal relaxing incisions. However, if necessary, astigmatism can be treated postoperatively with LRI or LASIK.
Consider providing "micro-monovision." The happiest patients are those with an outcome between -0.25 D and -0.5 D in one eye, and plano in the other.
Be alert for traditional IOL complications. As with monofocal IOLs, patients with the Array IOL can develop posterior capsule opacification. (Note: clinical studies have found no difference in surgical complications between multifocal and monofocal IOLs, although multifocal IOL patients may be more likely to experience halos or glare.)
Provide extra post-op counseling. Postoperatively, we help patients adjust to simultaneous vision. Patients may report distance blur, monocular diplopia, object glow, ghosting, or halos at night; most of these concerns are voiced during the first 60 to 120 days following surgery. We reassure patients that these symptoms usually disappear as the visual system adapts to the Array IOL. In some cases we prescribe brimonidine tartrate (Alphagan) or pilocarpine 0.5% at sundown to ameliorate the symptoms. (Only 0.5% of our patients report letting others drive for them because of problems with night glare.)
A Win-Win Situation
Our patients' outcomes with the Array IOL have been excellent. In 2001, we looked at the results of 1,454 bilateral Array implantations in cataract patients without other ocular pathologies, performed between 1998 and 2001:
- 94% of patients achieved distance UCVA of 20/40 or better; 59% achieved 20/25 or better.
- In terms of near UCVA, 91% of patients achieved 20/40 or better, and 40% achieved 20/25 or better.
- Of 591 patients who responded to questions regarding spectacle usage, 37% said they never used spectacles after the surgery; 57% said they used spectacles occasionally. Only 6% consistently used spectacles.
Offering the Array IOL has been a significant practice-builder for us. It's caused a dramatic increase in our surgical volume, which continues to grow. Over the next few years, I predict this will become the most frequently performed refractive procedure for patients over the age of 40.
Dr. Coffman has multiple offices and three ASCs in Palm Beach County, Fla., where he's been in practice for 30 years. He specializes in cataract and bifocal reduction surgery.
|
How the Array IOL Works |
The Array multifocal intraocular lens has five refractive zones. Zone 1 provides distance vision centrally, transitioning to intermediate vision peripherally. This provides the distance vision usually needed in bright light. Zones 3 and 5 are designed to be distance-dominant; zones 2 and 4 are near-dominant. The area between zones also provides some intermediate vision and a smooth transition between zones.
|
|
Accommodative IOLs Poised to Compete |
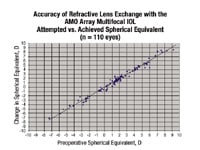
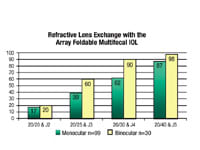
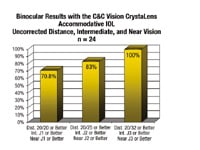
I was one of the original AMO Array Multifocal IOL investigators, so I've had more than a decade of experience with this technology. By and large it's been a happy and useful experience for me and my patients. Over the past several years, my partners and I have performed increasing numbers of refractive lens exchanges using the AMO Array Multifocal foldable IOL. Our results have been published, and they're very satisfying. Most of our patients have been hyperopic presbyopes, although increasingly we're implanting the lens in plain presbyopes. We're re-evaluating the data on myopes, based on the re-evaluation of Dr. Joseph Colin's patient population by Richard Packard from London. Because of the excellence of preoperative measurements and calculations using partial-coherence interferometry, and because of the availability of superb phacoemulsification technology, we've had spectacular accuracy in refractive lens exchange outcomes. (See "Accu-racy of Refractive Lens Exchange with the AMO Array Multifocal IOL," at right.) Also, in our early experience, almost all of our patients have been able to read and drive without glasses. (See "Refractive Lens Exchange with the Array Foldable Multifocal IOL," at right.) In our practice, 44% of the patients who have been binocularly implanted with the Array never wear glasses. Another 44% wear glasses on occasion, almost exclusively for prolonged reading or for driving at night, and about 12% wear them all the time (though not always because they're necessary). In addition to our experience with the Array, we've completed 25% of the FDA-monitored clinical study of the C&C Vision CrystaLens Accommodating IOL, and our experience with that lens has been outstanding. That lens is soon to be available for routine use here in America. In the clinical study, our data showed that of those patients in whom we did binocular implants, 100% were at least 20/30 at distance and J3 near and intermediate without correction, and 71% were at least 20/20 and J1. (See "Binocular Results with the C&C Vision CrystaLens Accommodative IOL," below.) Clinical trials have been conducted with an additional multifocal accommodating IOL, the HumanOptics IOL, in Europe, and four other companies have new innovative designs for other accommodative IOLs that will begin pre-clinical and clinical testing shortly. My belief is that, in spite of the great experience we've had with the AMO Multifocal IOL and others that look good based on early experience in clinical trials, accommodative IOLs will eventually win favor among patients and surgeons for the surgical correction of presbyopia. First, there have been no unwanted retinal images in our experience with the accommodative CrystaLens. Second, in spite of the small size of the optic, we haven't had any increase in complaints about glare or edge effects with these IOLs, compared with all other 6-mm-diameter optic monofocal IOLs. In addition, all multifocal IOLs achieve multifocality because of a division in the light, with portions of the light serving near vision, other intermediate, and the rest distant objects. The great advantage of accommodative IOLs is that all of the light reaching the retina will be coming from the object of regard, at whatever distance it is, because of the ability of the lens to move or change shape within the eye. Finally, because these IOLs don't require central nervous system adaptation, there will be no learning curve, and they will more naturally simulate the normal accommodation that all patients experience during their pre-presbyopic years.
|