LASIK and
Ocular Allergy
A growing number of refractive surgeons are taking into account the possible effects on outcomes.
BY LOUIS PILLA
Chances are that, as a refractive surgeon, ocular allergy doesn't rank high on your list of concerns when you evaluate a patient for LASIK. Yet, it's more than an annoyance. Left undiagnosed and untreated, it can cause a range of problems, and even affect your LASIK outcomes.
In this article, we'll reveal just how important diagnosing ocular allergy may be for your refractive surgery patient. We'll also discuss ways to uncover it, which don't require much extra chair time. First, though, let's look more closely at the problem's extent.

Perhaps your practice is "absolutely inundated with allergy," as Gary Luffey, M.D., Ruston, La., says is the case at his practice. He'll see ocular allergy in every third or fourth patient, he estimates.
Like many of his colleagues, admits Dr. Luffey, he sometimes won't pay enough attention to the problem. Patients, he notes, become used to mild hyperemia and low-level itching and don't consider it abnormal to have those conditions -- and aren't eager to bring them to the doctor's attention. Prior to LASIK, ocular allergy is probably underinterpreted, agrees Kerry Assil, M.D., medical director, Sinskey Eye Institute, Santa Monica, Calif.
Yet, ocular allergic conditions affect 20% to 25% of the general population, says refractive surgeon Francis S. Mah, M.D., assistant professor, department of ophthalmology at the University of Pittsburgh Medical Center, Eye & Ear Institute and co-medical director of the Charles T. Campbell Ophthalmic Microbiology Laboratory.
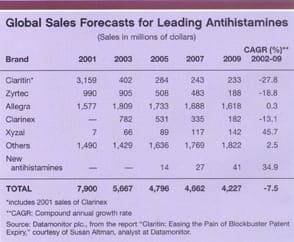
And although total sales for leading antihistamines are forecast to decline over the next few years, they still represent a more than $5 billion business this year, according to information from Datamonitor. (See "Global Sales Forecasts for Leading Antihistamines," on page 60.)
Allergy is even more common in younger patients -- very likely the ones coming to you for refractive surgery. What's more, patients may seek out refractive surgery because they're contact lens-intolerant, he notes. That means they may have some signs of allergy, such as giant papillary conjunctivitis or atopy. In addition, patients may not mention whether they use such over-the-counter (OTC) medications as Naphcon A or Visine. Many times, they won't consider those medications to be drugs, notes Dr. Mah.
Range of Difficulties
Ocular allergy can lead to a range of problems, notes Dr. Assil. In the short term, for instance, mechanical eye rubbing can cause slipped flaps, striae, and epithelial ingrowth in LASIK patients. In the long term, it can cause flap margin fibrosis.
In a recent study, Stephen Boorstein, M.D., associate director of refractive surgery at Davis Duehr Dean Centers for Refractive Surgery in Madison, Wis., found a higher incidence of diffuse lamellar keratitis (DLK) in patients with atopy.
Instead of looking for an exogenous cause, Dr. Boorstein, who is also clinical associate professor at the University of Wisconsin, attempted to discover patient-specific factors. In a retrospective study of patients who had bilateral myopic astigmatic primary LASIK, he discovered that those patients with atopy were 5 times more likely to exhibit DLK than those with no atopy.
What's more, he found that the risk declined to the same level as a nonatopic patient when the atopic patient took a nonsedating antihistamine. Most likely, he notes, the medication was doing something immunologic to decrease the risk.
Similarly, Scott MacRae, M.D., professor of ophthalmology at the University of Rochester, studied 13 eyes of 13 patients who developed DLK after LASIK. Six patients (46%) had a history of severe seasonal allergies, atopy, and asthma, he noted in the Journal of Cataract and Refractive Surgery.
With patients less likely to bring up ocular allergy as a concern prior to refractive surgery, you'll need to stay alert to the condition. Just asking about allergies won't do the job, says Dr. Assil.
Patients, he says, tend to think of allergies in terms of such rhinitis-type symptoms as runny nose and sneezing. And they may get defensive if you ask whether they rub their eyes. Instead, ask if their eyes itch, he recommends.
Patient history also plays an important role, notes Dr. Luffey. Ocular allergies, he says, involve not only physical but historical findings as well.
Note, says Dr. Assil, that many patients with allergies will also have other external disease components, such as dry eye, blepharitis, or meibomitis. The "three conditions seem to quite often run in a triad," he says.
Treatment Options
Treating ocular allergy is part of ensuring that the eye is quiet prior to refractive surgery. The goal, says Dr. Luffey, is not only to relieve symptoms, but also to address the underlying inflammatory process.
On diagnosing ocular allergy, Dr. Assil immediately starts prophylaxis with an allergy drop. For severe exacerbations, he'll periodically add FML topical steroid.
If a patient is already taking an oral antihistamine, Dr. Assil won't necessarily have the patient stop that medication (if he perceives a nonfocal, systemic allergy), but it doesn't necessarily cover "the focal allergic conjunctivitis as well as the topical drops," he says. For a patient with systemic allergies, stopping the oral medication doesn't make sense "but if it's just confined to allergic conjunctivitis or allergic rhinitis, then switching may make sense."
Using a somewhat different approach, Dr. Mah will change the patient over from an oral antihistamine to a topical medication. The reason for the switch to a topical medication is evidence-based, according to Dr. Mah. Several papers, he notes, have documented the corneal drying effects of antihistamines.
Because LASIK and other keratorefractive procedures cause a temporary neurotrophism with associated dry eyes, anything that can be done to minimize dry eyes would benefit these patients, notes Dr. Mah. Furthermore, he says, loratadine, a systemic antihistamine, has been shown to delay epithelial healing following PRK.
Postoperatively, he'll normally keep the patient on the topical agent. If that doesn't control the systemic component of the allergies, he may add Flonase (or another nasal steroid) before putting patients back on an oral medication, though usually the drop is enough.
Prior to LASIK -- and cataract surgery -- Dr. Luffey recommends a multi-action allergy drop. This provides both an antihistamine and mast-cell stabilizing effect, and inhibits other inflammatory mediators, which are perhaps a less well-defined part of ocular allergy. He keeps patients on the drops postoperatively, as well.
Dr. Boorstein, too, treats patients who have allergies and exhibit signs and symptoms before refractive surgery. He'll be conducting a placebo-controlled trial to determine whether atopic patients who are more prone to environmental allergy may benefit from being started on nonsedating antihistamine drops or oral treatment even if they don't exhibit allergy signs and symptoms.
Physicians should discourage the use of OTC treatments, notes Dr. Luffey, which he says are loaded with preservative and can cause rebound vasodilation of the conjunctival vessels with potential loss of vessel muscle tone. Instead, he recommends the use of ocular allergy medications. And artificial tears, he notes, are an excellent OTC addition to prescription treatments.
Next Frontier
Wavefront technology may add even more weight to addressing ocular allergy. Wavefront-guided surgery, says Dr. Boorstein, depends on removing corneal tissue in a specific pattern for each individual with micron accuracy; the healing response could affect this treatment.
Anything that might help clinicians understand and guide healing could be important to this process. "This may be the next frontier in refractive surgery in understanding outcome," he notes.
Pilla (louispilla@comcast.net) is a freelance healthcare journalist based near Philadelphia, Pa.
|
Ocular Allergy: Just Ask the Question |
If you're not asking patients whether they suffer from ocular allergies, you're missing an opportunity to provide relief for a widespread condition. Discovering whether your patient has ocular allergy doesn't involve complex clinical tests. Rather, it's a matter of simply asking the right questions. Last year, 41 million bottles of OTC eye drops for allergies were bought, compared with 4 million prescriptions, says Joseph F. Mussoline, M.D., clinical instructor/assistant surgeon at Wills Eye Hospital, Philadelphia, Pa. "That tells you right away that we're failing to ask the question about allergies," he asserts. With a wet winter and then blistering summer heat as well as a high pollen count in the Philadelphia region, he's gotten in the habit of asking patients about any itching, burning, or redness. He estimates he writes about 25 to 30 allergy prescriptions per week, compared with the one or two each week he'd write if he didn't ask the question. On Long Island, N.Y., the story is much the same for Jodi Luchs, M.D., at South Shore Eye Care. While the incidence of allergy depends on factors such as weather and pollen, he estimates that if he sees 50 patients per day, it's not uncommon that 10 to 15 of them complain of ocular allergy symptoms as all or part of their chief complaint. Because allergies are so widespread, Dr. Luchs hopes to incorporate a few key questions in his patient history to streamline the history-taking process and obtain information about allergies. Dr. Luchs stresses the need to distinguish patients who suffer from fleeting allergies versus those whose conditions are chronic. While medications such as Visine might treat fleeting symptoms, it's a "Band-Aid type of treatment" that doesn't affect the chronic allergic inflammatory cascade, he says. If you take the time to ask about allergies and treat the patient with a more comprehensive product, he says, you can break the cycle of symptoms, treatments, return of symptoms, emergency phone calls and visits that might otherwise result. Jacqueline Dauhajre, M.D., based in Manhattan and Queens, N.Y., specifically asks patients if they have itching, burning, or tearing. If the patient says no, she doesn't stop there. Instead, she asks if the patient uses drops like Visine. Some 25% of patients who say they have no symptoms use Visine, she says. For those with severe allergy, she'll mix a topical prescription drop with a soft steroid. Then, she'll wean the patient from the steroid and maintain the allergy drop. Make sure you ask the patient about allergies, Dr. Dauhajre recommends. It "takes two seconds." |








