Switching to
Immersion Biometry
The reasons to change are compelling. Here are five steps to ensure it's a smooth transition.
BY RHONDA G. WALDRON, MMSC, COMT, CRA, ROUB, RDMS
Today, patients expect cataract surgery to not only restore visual clarity, but to provide excellent vision in refractive terms as well. Unfortunately, the commonly used method of contact biometry isn't accurate enough to produce outcomes that live up to these expectations. The only way biometry technicians can obtain consistent, accurate, reliable readings is by eliminating the error induced by corneal compression.
Surgeons have relied on the applanation technique for years, and most have personalized their IOL constants to try to counteract the corneal compression error. However, no one disputes that immersion ultrasound is the gold standard of biometry. (In fact, the IOLMaster, which has also proven to be extremely accurate, was calibrated to immersion ultrasound.)
So why don't more practices use it? Part of the problem is that making the switch can be a little frightening; doctors are concerned that the change will require expensive equipment and a great deal of staff training.
In fact, this isn't the case.
Setting the Record Straight
Besides the unquestioned accuracy of immersion biometry, there are other good reasons to switch from applanation biometry:
Immersion biometry is faster and easier. A common misconception is that immersion is more difficult to perform and more time-consuming for the technician. Actually, the opposite is true; immersion biometry is easier than the contact method, and it takes a fraction of the time to perform. This means that a technician using immersion biometry is not only more accurate but also more efficient.
|
|
|
|
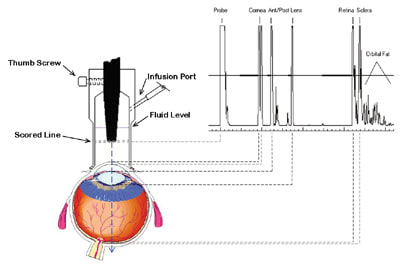
During immersion biometry, visual axis alignment is easier to achieve using an infusion shell; the probe is locked into the center of the shell |
|
The immersion technique is quite simple. The technician gently places a small scleral shell on the anesthetized limbus; the probe is either hand-held within the fluid, or locked into position in an infusion shell. (See the illustration at left.) The fluid is infused into the shell through tubing that connects the shell to either a bottle of BSS or a 5-cc syringe of contact lens saline. (Infusion scleral shells can be used with the patient sitting upright, but it's easier for both patient and technician if the patient reclines.)
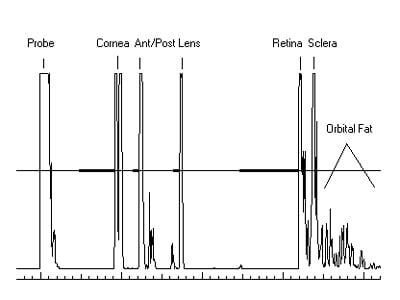
When the probe is aligned along the visual axis, five tall spikes are clearly visible in the scan (representing echoes from the cornea, anterior lens, posterior lens, retina and sclera) with the retinal spike rising steeply from baseline. The corneal spike is separate from the probe spike and has a double peak, representing the epithelial and endothelial layers of the cornea. (See the close-up of a scan, above.)
Measurements made by different technicians will agree. Because immersion biometry eliminates the corneal compression factor, it also eliminates the problem of having to depend on one particular biometry technician. All measurements will be within hundredths of a millimeter of each other, as long as the technician aligns the probe with the visual axis.
Applanation biometry may limit next-generation IOL access. Another reason to switch to immersion is the development of multifocal IOL technologies and accommodating IOLs such as the CrystaLens from eyeonics, inc. (formerly C&C Vision). According to J. Stuart Cumming, M.D., this lens will only be available to those practices that use non-contact biometry -- either immersion ultrasound or optical coherence biometry. (For more on this, see "Accurate Biometry is Crucial for New IOLs".)
|
|
|
|
To minimize errors and ensure visual axis alignment, an
immersion biometry unit should show tall, straight spikes of equal height, with good resolution of the corneal peaks and
retinal/scleral spikes. |
While the IOLMaster can match the accuracy and efficiency of immersion ultrasound, it's an expensive instrument. Also, it can't be used when patients are unable to fixate or have dense cataracts or other media opacities. Immersion ultrasound is a more cost-effective alternative that can be used with all patients, regardless of cataract density or visual acuity level. (Even practices that use the IOLMaster will continue to need immersion ultrasound for patients who can't be measured using optical coherence biometry.)
Immersion also provides an accurate measurement of lens thickness and anterior chamber depth, which are needed for current fourth-generation formulas.
Making the Switch
Once you've decided that your practice should switch to immersion biometry, taking these five steps will help you make a smooth transition:
Obtain quality equipment. High-quality immersion ultrasound units are now available for $5,000 to $7,000. But be careful: Although most equipment of this type is similar in cost, it's not all of equal quality. To get a unit that will produce the best results:
► Make sure the display screen shows tall, straight spikes of equal height, with good resolution of the corneal peaks and retinal and scleral spikes. Units that can't display straight spikes or haven't properly compensated for sound attenuation make perpendicularity errors much more difficult to detect. They also make it impossible to be sure of visual axis alignment.
► Be certain that the four gates, or calipers, are visible --and moveable -- in both automatic and manual modes. You should be able to verify exact measuring points for the anterior chamber depth, lens thickness, and vitreous chamber length, and be able to move the calipers when they're incorrectly placed. (All units will occasionally place a gate at the wrong measuring point -- for example, when a dense cataract causes multiple spikes between the anterior and posterior lens echoes.)
► Look for a machine that measures each section of the eye (anterior chamber depth, lens thickness, and vitreous cavity) at its individual sound velocity, and then adds them together for the total eye length measurement. Units that use average velocity from the cornea to the retina will produce inaccurate measurements, particularly in a short eye.
► Make sure you can adjust the gain setting. Cataract density varies, and the amount of gain you need will change accordingly.
► Only buy a unit that you're allowed to use on a trial basis first. Also, ask for a scleral shell to be included, so you can use the immersion technique during the trial period.
► Make sure you and your biometry staff read the equipment manual thoroughly. The newer, more sophisticated units have more type-of-eye settings and more controls, so you'll need to learn not only how to use the unit, but also what features and options are available.
Purchase an immersion scleral shell, if one isn't included with the unit. The cup-style shells (such as the Hansen or Ossoinig shell) are inexpensive, but they involve a longer learning curve for your staff. Infusion shells (such as the Prager or Kohn shell) are a bit more expensive, but they're much easier to learn to use; visual axis alignment is easier to achieve because the probe is locked into the center of the shell. If the shell is placed flush with the limbus, visual axis alignment is achieved almost immediately.
Infusion shells are designed to fit specific probe diameters and sizes, so be sure to name the biometer manufacturer and model when ordering, or simply order it directly from your ultrasound equipment manufacturer.
Invest in one day of training for all technical staff. That's all it takes -- one day. Either have all technicians (and, if possible, all surgeons) attend a one-day seminar that includes hands-on training, or have an immersion expert come to your office.
To provide good patient care, your technicians need to be experienced at:
► immersion technique
► spike pattern interpretation
► correlating measurements to the patient's refractive system
► problem-solving anomalous waveforms
► handling challenging cases such as the post-refractive surgery patient and the high myope.
Also, certified technicians need continuing education credit hours, so be sure the seminar is JCAHPO-accredited. In addition, consider getting all biometry staff certified in ultrasound biometry by having them take the Registered Ophthalmic Ultrasound Biometrist (ROUB) examination offered by the American Registry of Diagnostic Medical Sonographers.
Design an ergonomic biometry exam room. This measurement is critical, and the space allocated for the procedure should reflect this. It shouldn't be cramped and uncomfortable. To ensure consistent results:
► Provide a reclineable chair for the patient. Having the patient sit upright is more awkward for both the patient and the examiner.
► Be sure to place the machine within easy view and reach of the biometrist.
► Have a fixation target carefully positioned on the ceiling.
Re-personalize your lens constants. Because the immersion method produces slightly longer eye lengths than the contact method, you'll need to increase your constant to avoid slightly hyperopic post-operative surprises. Studies have shown that, on average, eyes measure anywhere from .14 to .36 mm longer when using immersion biometry. Some surgeons suggest adding about 0.3 to the constant you previously personalized for the contact method.
According to Jack T. Holladay, M.D., the best method is probably to measure the first 20 or 30 patients using both the contact and immersion techniques. Once you find the average difference between the two measurements, simply double the number and increase your constant by that amount. For example, if the average difference in length between the contact and immersion methods is 0.2 mm, add 0.4 to the constant.
Once you've measured 20 or 30 patients using only immersion and the new constant, you can refine it further.
Accuracy and Efficiency
Immersion ultrasound truly is the gold standard in biometry. It provides the efficiency and accuracy you need to achieve the standardized, high-quality postoperative results that today's cataract surgeons and patients demand. Making the switch is easier than you think, and doing so will help you provide your patients with the level of care they deserve.
Rhonda Waldron is the diagnostic echographer and senior associate in ophthalmology at Emory Eye Center at Emory University in Atlanta. She also owns Eye Scan Consulting, and teaches both A-scan and B-scan ultrasound across the country and in Europe. You can contact Ms. Waldron at rwaldro@emory.edu.
|
Accurate Biometry is Crucial for New
IOLs |
One of the latest technological advances in cataract surgery is the development of IOLs that allow patients to see at near and distance (or at all distances) without glasses -- or at least be much less dependent upon glasses than they would have been with standard lenses. For best results with these multifocal and accommodating lens designs, patients need excellent uncorrected distance vision with a refraction close to emmetropia. This has greatly contributed to the importance of performing accurate biometry and keratometry. The most common method of measuring axial length is by the applanation technique. However, unless this is done by a highly skilled technician, it tends to produce myopic surprises because of indentation of the cornea. It's rapidly becoming apparent that the most accurate way to measure axial length is with Carl Zeiss Meditec's IOLMaster using the third-generation software or by immersion biometry. Using these methods with the appropriate "A" constant and a modern formula, it's possible to get results that are consistently within .5 diopters of the anticipated postoperative refraction. The IOLMaster is extremely user-friendly because there's absolutely no contact with the eye. Some practices have ultrasonic equipment and prefer to use immersion biometry. Immersion biometry has also changed dramatically, thanks to the development of the Prager Shell (created by Thomas Prager, Ph.D). The shell is applied to the eye after a local anesthetic, and the biometry can be done with the patient in a semi-reclined position using less than 2 cc of BSS. There has been some resistance to using this technique because many practices have been using the applanation method for so long. However, once doctors and technicians get used to immersion biometry using the Prager Shell, they find that it's much quicker and far more accurate than the applanation method. I believe that any surgeon who wishes to produce excellent distance vision for patients with accommodating or multifocal lenses should switch as soon as possible to the IOLMaster or immersion biometry for axial length measurements. In addition, K readings are best taken from the IOLMaster or done manually. Once doctors and technicians are able to obtain excellent uncorrected vision with standard lenses, they will then have prepared their practice for the new class of lenses, which will enable their patients to either go without -- or greatly reduce their need for -- glasses. Using the recommended "A" constant and the appropriate modern formulas, there should be no need to make any significant adjustments or use so-called "fudge factors" to get good results. Dr. Cumming is the inventor of the CrystaLens accommodative IOL and chief scientific officer for eyeonics, inc. (formerly C&C Vision). |