Glaucoma
Case Studies
Diagnosing and Treating Epithelial Downgrowth
BY ROBERT J. NOECKER M.D., LISA A. HERRYGERS M.D., AND JASON M. LEVINE
M.D.
Case history/presentation: A 45-year-old male was referred to our glaucoma clinic with IOP in his right eye in the 40s, despite maximum topical medical therapy (latanoprost [Xalatan], dorzolomide and timolol [Cosopt] and brimonidine tartrate [Alphagan]). He complained of blurry vision and a dull, aching pain.
One year earlier, the patient had undergone extracapsular cataract extraction. Prior to that surgery, he'd been highly myopic (-12D). After surgery, his IOP was 8 mm Hg with anterior chamber inflammation. Dynamic Seidel testing revealed a wound leak; the IOL was dislocated as well. The surgeon performed a lens exchange and revised the wound in an attempt to stop the leak.
Over the course of several months, the patient developed chronic inflammation and his IOP increased. The doctor prescribed several glaucoma medications, but the patient's IOP remained in the 40s. Eventually the patient was referred to our glaucoma clinic for further IOP management.
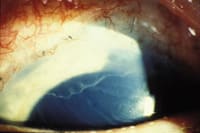
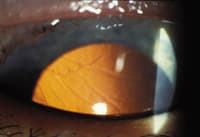
Examination: Examination revealed a peripheral retrocorneal membrane on the superior cornea. (See photographs, below.) Gonioscopy revealed epithelialization of the angle and formation of peripheral anterior synechiae (PAS). The diagnosis of epithelial downgrowth was confirmed with argon laser photocoagulation.
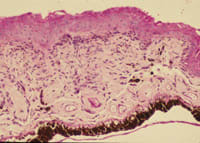
Treatment: We applied cryotherapy to the affected cornea and angle, and then surgically excised the affected iris and performed an anterior vitrectomy. Histologic examination of the excised iris confirmed the diagnosis of epithelial downgrowth. (See photograph, following page.)
|
|
| Left: A slit lamp photo of the superior cornea demonstrates a scalloped, gray line representing the multicellular, thicker leading edge of the epithelial sheet. Right: Retroillumination of the superior cornea shows the thickened leading edge of the posterior corneal epithelial layer. | |
Discussion: Epithelial downgrowth is a rare complication of intraocular surgery. It's been reported following trauma, penetrating keratoplasty, glaucoma filtering surgery and cataract extraction. Here's a brief summary of what we know about this condition:
Causal factors. Researchers believe that epithelium gains access to the anterior chamber through poor wound apposition with incarcerated tissue serving as a wick; hypotony is often present initially. Inflammation may also play a role by providing the proliferating epithelium with nutrients as well as altering wound healing, leading to fistula formation.
Glaucoma occurs because of the epithelialization of the trabecular meshwork, the development of PAS following prolonged hypotony and inflammation, as well as possible pupillary block. IOP is often resistant to treatment with topical glaucoma medications.
Incidence. Modern surgical techniques have decreased the incidence of this complication dramatically; the last retrospective review, published in 1989, estimated that this complication occurred in less than 0.08% of surgeries. The incidence is now thought to be even lower.
Currently, the literature contains three reports of epithelial downgrowth following clear corneal phacoemulsification, four cases following Molteno implant surgery and one case following Ahmed implant surgery. Several surgeons have reported instances of epithelial downgrowth following keratoplasty.
Common elements at presentation. Patients with this condition usually present within the first year after surgery, but they may present anywhere from 4 days to more than 10 years after the triggering event. Generally:
- The typical patient is young and highly myopic or diabetic.
- The most common presenting symptoms are decreased visual acuity, red eye and pain.
- The most common presenting signs, according to a 30-year retrospective review by Weiner et al., are retrocorneal membrane (45%), glaucoma (43%), corneal edema (21%), and a positive Seidel test (23%).
- Gonioscopy often reveals incarceration of iris, lens cortex or capsule, or vitreous in the wound, as well as PAS.
|
|
|
|
Histologic specimen of resected iris demonstrates epithelial growth on the posterior surface of the iris
(hematoxylin and eosin).Place ad here and delete rule: |
Tests to establish diagnosis. Diagnostic tests that are helpful for establishing the diagnosis of epithelial downgrowth are dynamic Seidel testing, specular microscopy, argon laser photocoagulation, iris biopsy, anterior chamber curettage, aqueous aspiration and diagnostic vitrectomy.
Treatment. The mainstay of treatment is surgical removal of epithelial downgrowth and closure of any wound fistula. Injecting antimetabolites such as 5-FU has produced limited success.
Typically, treatment consists of argon laser photocoagulation to define the extent of epithelial involvement, en-bloc excision of involved iris and/or ciliary body (or iris excision with vitrectomy), anterior vitrectomy and fistula closure. Cryotherapy is then applied to the involved cornea and sclera.
Although epithelial downgrowth is rarely seen in clinical practice today, when it does appear, early diagnosis and treatment can result in improved outcomes.