Ramping Up for
Custom Ablation
Part Three: Impact on patient flow.
BY DESIREE IFFT, EXECUTIVE EDITOR
The maker of a special-ordered luxury car spends more time and uses more resources to create his product than does the maker of a more basic model. His process is different because his goals are different. He wants to provide each customer with the car that best suits that customer's individual needs. In turn, what his customers are willing to pay for their cars will reflect the value he's added.
To help you plan effectively for your move into custom procedures, we sought advice on key patient flow and processing elements from international surgeons who already have some experience and consultants who are helping practices prepare.
Preoperative Testing
Capturing a patient's aberrometry data and entering it into treatment calculation software are the extra pre-op steps required for custom procedures. The time needed can be anywhere from 10 minutes to 45 minutes per case.
"Just like with topography," says Michael Lawless, M.D., of New South Wales, Australia, "you have to make sure the patient is blinking properly, has a good tear film, is looking in the right place, and that the eye is autofogged to minimize accommodation."
Multiple scans are taken and must be compared with traditional refraction data to ensure the two sets of results are not significantly different. In some cases, scans may need to be retaken. Taking the measurements becomes routine with experience, and newer versions of software help in selecting the best map, on which the ablation will be based.
Staff need the necessary training to operate the new device, Dr. Lawless says. And all members of a practice team need to be highly educated in the custom environment.
That's the relatively straightforward part, which is similar among all platforms. What varies among them is whether or not the patient's pupil must be dilated for you to capture his wavefront measurement and whether his pupil then needs to be dilated or undilated for treatment. If your system requires dilation for either phase, you will need to decide where to build in that extra time, on the patient's consult day or his treatment day.
Gordon Balazsi, M.D., of Montreal, has been performing custom procedures on two platforms, Zyoptix from Bausch & Lomb and CustomCornea from Alcon. On the B&L system, patients are dilated for wavefront measurement, but not for treatment. So, on that system, he does a patient's image capture and treatment on different days.
"With the B&L system, you can't test the wavefront after anesthetic drops have been used to take a pressure, so our patients see a refractive counselor first," explains Dr. Balazsi. "Next, they're screened by an optometrist to make sure they're a reasonable candidate for a custom procedure. Then we dilate them and take their wavefront measurement. If everything checks out OK, they go back to the O.D. for a pressure check and fundus exam. Then they see the ophthalmologist. They return on a subsequent day for treatment. So, there are a lot of steps on the path that have been added or rearranged because of the need to measure the wavefront dilated."
On the Alcon system, wavefront image capture and treatment are both performed on dilated pupils. In this scenario in Dr. Lawless' practice, surgery day is the patient's first wavefront measurement. "Before we began custom treatments, we took diagnostic wavefronts on a good number of patients and found that the readings are very reliable," he says. "If that weren't the case, and the technology wasn't as robust as people said it would be, then we would be performing the test ahead of time. But we were confident in eliminating that step. Therefore, our patients don't have a LADARWave taken at the time of the consultation."
That means the workup process is really no different than with standard LASIK. "When it's time for surgery is when the patient flow issues come into play," he says. "First, in order to center the treatment, an undilated centration image is taken at the LADARWave. Then, we dilate the patient and capture the wavefront. Dilation for the wavefront reading must be out to at least 6.5 to 7 mm, which takes 15 minutes to a half hour. When the desired wavefront image is obtained, the technician marks the limbus with ink to help in the registration process. Then, the patient is taken into the laser suite to be treated."
Between wavefront capture and treatment, the ablation plan must be created. On each of the several platforms, this is accomplished with a combination of software calculations, surgeon input and technician data entry. The extent of allowable surgeon input will vary depending on how much flexibility a platform's FDA approval entails.
Senior technician Dominique Matte describes how the treatment plan calculation is handled in Dr. Balazsi's practice: "Once we obtain the corneal and wavefront scans, we print them out for the doctor to review. He writes his desired adjustments on the sheets; the changes are entered into the computer by a technician; the final plan is calculated by the computer and copied to a disk, which, on treatment day, is put into the laser computer."
Matte estimates that the entire pre-op data process, including taking measurements and entering numbers, takes an average of 30 minutes per case. So, for patients undergoing custom LASIK workups, the scheduling desk books what would have been two standard LASIK time slots.
Joel Nunneley, Managing Principal of Client and Creative Services for Medical Consulting Group in Springfield, Mo., says practices will likely spend about an hour and a half with custom patients. "Depending on the technology platform being used, and other practice-specific factors such as staffing levels, some centers may be able to pare that down," he says. "So, as a general rule of thumb, count on spending 50% more time with custom patients than with standard LASIK patients. That's a good starting point for planning."
Finding Ways to Maximize Efficiency
Regardless of what platform you're using and its dilation requirements, the bottom line is that aberrometry and treatment plan calculation will have to be worked into your patient flow process. Heather Ready, Director of Business Development for VISX, recommends that before you figure out where to add the necessary steps to your process, you sit down and define your current process. What tests do you perform now? How does your patient move from A to B to C. "Based on your situation, you can decide where it makes the most sense to integrate your aberrometry testing."
She also recommends standardizing among your doctors what tests are performed and in what order. "Move the patient as few times as possible from room to room," says Ready. "If you can have more than one refractive-surgery-related test in one room, that's good."
If your refractive patients move through the practice with other patients, avoid having unrelated exams that take more time in the same room. "You don't want to have to interrupt a room where a visual field is being done, or wait until that room is not in use to have access to your aberrometer. Eliminate the starts and stops as much as possible."
Arturo Chayet, M.D., Tijuana, Mexico, has performed 350 custom procedures, beginning in late 2000 with clinical trials for the Nidek NAVEX platform. He's been providing treatments for patients outside the trials for about 4 months now. "At first, it was a little hectic," he says. "But now the staff is used to it and it's part of the normal flow."
About 70% of his refractive patients undergo a custom workup with the OPD-Scan, which does not require dilation. Because treatment with NAVEX doesn't either, he does most workups and treatments on the same day. Per custom case, it takes his team about 5 additional minutes to capture OPD-Scans in the clinic, 10 additional minutes entering data for treatment plan calculation, and 3 additional minutes working with the data in the OR.
One change Dr. Chayet made to save time was bringing a laptop computer with access to the calculation software into the OR to handle any final treatment plan adjustments prior to surgery. "Before that, we would have to go back and forth between the clinic and the OR," he says.
His practice has also designated one person to handle all of the aberrometry data. This is best for consistency and flow, Dr. Chayet says. Also, that person can enter data for several cases into the treatment calculation software at the end or beginning of the day.
Patient Education
Patient education is the second key element that affects flow in a practice that offers custom procedures. Once a practice decides to offer both standard and custom LASIK, it is dealing with a menu of options, says Mark Danzo, CEO and president of Danzo International, a refractive-focused consulting company in Colorado Springs, Colo.
"Before, it was just are you a candidate or are you not a candidate," he explains. "But now there really is a selling process that has to take place in conjunction with the candidacy process. To raise its average fee sufficiently to provide custom LASIK, a practice has to be proactive about presenting it to every patient for whom it's appropriate."
"Therefore," Danzo says, "practices must commit to a carved-out education session during which they discuss with prospects the advantages of custom, why it's better for them, and why it's worth paying X amount. Otherwise, they won't choose it."
The session, he continues, "should not take place across the wavefront unit. It should be conducted by a refractive coordinator, not a tech or a surgeon, and it should be done before the clinical process. Why qualify patients medically if they don't understand the benefits enough to make the choice? It's a waste of chair time."
Dr. Balazsi learned firsthand the importance of who handles the patient education. At first, technicians were doubling as counselors. "That became a bit heavy," he says. "And it wasn't the best use of our highly qualified techs' time." They're now in the process of separating those two tasks and hiring two or three new counselors.
Nunneley agrees that a practice's commitment to patient education is crucial to smooth patient flow. "Plant the seed early and often," he advises. "The person answering your phones should always ask callers whether they've heard of customized ablation. Nine times out of 10, they'll say no, so direct them to your Web site where they can begin to familiarize themselves with the new customized concept, and tell them you'll talk with them about it when they come in.
"As soon as patients are checked in, hand them a brochure about custom LASIK to read while they wait for the refractive coordinator. Once the technician comes in and begins the diagnostic testing, employ what I call 'test and teach.' As you go through the process, explain it in layman's terms: each eye is unique, that's what you're measuring, and this is why it's important to your treatment."
Nunneley says it's important for everyone in the practice who comes in contact with refractive patients to convey the same message and use the same terminology to describe custom LASIK. He also advises practices to role-play through their education process to see how it comes across. Does it make sense, feel comfortable, sound like something of value?
He's found that practices who were waiting to educate until the doctor was in the exam lane with the patient were not doing well converting patients to custom LASIK. "The critical question patients have for their doctor is whether he or she would make the same decision for his or her own eyes," Nunneley says. "The doctor doesn't really have to sell, other than believing in the value of the technology and making the recommendation.
"If he or she is the one popping this new information onto patients, the conversion rate will go down. This is a once-in-a-lifetime decision, and patients don't want to make it on the spot. The wrong approach can take a certified, ready-to-jump-in-with-both-feet LASIK patient and put him back on the fence. It also turns your doctor into a refractive coordinator. If a patient asks him or her 'Zyoptix, what's that?' or 'WavePrint, what's that?' instead of a 10-minute exam, you've got a 30-minute sales session, and you're backed up all day."
Think of it as a Second Chance
One of Dr. Chayet's main goals from the start was to prevent patient confusion over technology. Therefore, he decides which patients are good candidates for custom and matter-of-factly lets them know that he thinks it's the best approach for their eyes.
"If we're always telling them there's something new, they postpone having the procedure in favor of waiting for perfection," he says. "Confusion is the worst thing that could happen right now for the whole industry."
The worst thing indeed, especially because custom is a much-needed chance to reinvigorate refractive surgery.
THE SCHWIND APPROACH
Early Work Shows Safety
and Efficacy
BY MARIA CLARA ARBELAEZ, M.D.
|
|
|
|
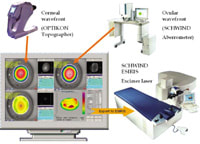
The Schwind custom ablation platform uses topography and wavefront measurements to drive treatments. |
|
Today's ophthalmology clinics must be ready to meet high patient-satisfaction demands. In refractive surgery, we have to achieve excellent outcomes with respect to visual acuity and night vision. We must also strive to make induced aberrations obsolete and to offer patients with unsatisfactory outcomes after earlier treatments a new perspective.
Technology advances in the past 5 years have brought us much closer to these goals. We now have the wavefront aberrometer, which allows us to measure higher-order aberrations. And excimer laser parameters are much different from the mid-1990s. We have Gaussian beam profiles that don't exceed 0.8 mm in diameter; we have high repetition rates; we can achieve smooth ablation surfaces without ablating too much tissue; and we have precise, reliable and fast-responding eye trackers.
Technical Requirements
|
|
|
|
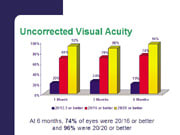
Change in patients' best-corrected visual acuity following custom treatment with the Schwind approach. |
The Schwind approach to measuring and customizing treatments to individual eyes includes the Schwind aberrometer, which is a Tscherning-type aberrometer, the Optikon Scout topographer, the Schwind ORK software, and the Schwind Esiris scanning spot excimer laser.
The platform uses both information about the anterior cornea surface, measured with the topographer, and the total ocular wavefront, measured with the aberrometer. (Approximately 80% of aberrations are related to the cornea, especially for patients who have had a former refractive laser treatment.) The advantage is the ability to describe the irregularities of the anterior cornea surface in terms of corneal wavefront up to the 7th order of Zernike polynomials and compare them with the ocular wavefront.
With this diagnostic information, and the help of simulating patients' point spread function under different lighting conditions and pupil diameters, the surgeon is able to determine which problems affect each patient's vision the most.
|
|
|
|
Prior to treatment, none of these patients was seeing better than 20/30 uncorrected; 1 month postoperatively, 60% of patients had uncorrected visual acuity between 20/20 and 20/25. |
|
The ORK software is the link between diagnosis and treatment. It translates patients' individual wavefront error into the customized ablation pattern to be treated by the laser. It is designed not only to perform sphero-cylindrical treatment, but also to reduce aberrations such as coma, spherical aberration and higher-order astigmatism.
Early Experience
Based on corneal wavefront technology with the Schwind ORK Software and the Esiris laser, we treated a group of 18 eyes with corneal irregularities. The preoperative refractive range was from +5.00 to -5.00 of sphere with astigmatism up to +6.00D.
Twelve patients were observed at 1 month follow-up. Postoperative best-corrected visual acuity was improved compared with preoperative BCVA:
- 25 % of patients gained one line of BCVA
- 8% gained two lines
- no patient lost more than one line of BCVA.
Preoperatively, no patient was seeing better than 20/30 uncorrected; 1 month postoperatively, 60% of patients had uncorrected visual acuity between 20/20 and 20/25.
|
|
|
|
After a previous refractive treatment, this undercorrected patient complained of double vision and severe problems while reading. Pictured here are his preoperative (a) and postoperative (b) corneal topography maps, difference map (c) and the
Schwind/ORK customized ablation pattern
used for his re-treatment. Treatment resulted in a stable refraction, 20/20 uncorrected acuity and elimination of
his complaints. |
Solving a Problem from Previous Surgery
In one case, a 42-year-old patient underwent a procedure with a laser other than the Schwind Esiris to correct a 6.00D 1.75D x 175 refractive error. Ten months post-op, the patient complained of double vision and severe problems while reading. His refraction was +1D 1D x 180. The eye was overcorrected, showing induced spherical aberrations because of a too-small optical zone, which explains the symptoms.
To improve the patient's vision, customized corneal correction with the Schwind ORK corneal wavefront platform was planned. (See image below.) The approach was to increase the optical zone, decrease spherical aberration, and reduce the previous overcorrection to 0.75D of monovision to improve the patient's reading ability. This approach was successful. The target was achieved. Treatment resulted in a stable refraction, 20/20 uncorrected acuity and elimination of his complaints. Re-treatments with the help of customized correction will be a significant portion of future practice.
Technology is Only One Factor
While these results are encouraging, many questions about custom procedures have yet to be answered. For example, will it be LASIK, LASEK or perhaps PRK that will allow us to achieve the best possible results?
And even the most advanced technology is no guarantee for excellent results. Surgeons must strictly plan and manage each procedure to obtain predictable results and good quality of vision for patients.
Also, the personnel in our clinics must be skilled and trained to understand and believe in the new technology and the advantages it provides. Prospective patients use all types of sources of information about customized refractive correction and expect a high standard of knowledge by the office staff as they perform the necessary diagnostic tests.
Dr. Arbelaez is a refractive surgeon at the Muscat Eye Laser Center in Oman.
THE VISX WAVESCAN WAVEFRONT SYSTEM
6-Month Clinical Trial Produces
Compelling Results
BY COLMAN KRAFF, M.D.
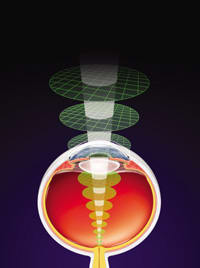
Results from the first 6 months of a multicenter FDA clinical trial for wavefront-guided LASIK using the VISX WaveScan Wavefront System demonstrate that the procedure is highly accurate, predictable, and safe for the treatment of patients with low to moderate myopia with or without astigmatism.
All patients in the 6-month cohort received bilateral treatments using one of three microkeratomes, the Moria, Amadeus, or Hansatome. Otherwise, the surgical technique was standardized -- with no nomogram adjustment. All eyes were targeted for emmetropia. The custom ablation zone was out to 8 mm, and there was very tight control in terms of environmental conditions, such as humidity and temperature.
One of the unique aspects of the VISX wavefront clinical trial is the use of the PreVue Lens system for preoperative screening. The PreVue Lens can identify those patients who may benefit the most from a wavefront correction by measuring their potential improvement in BCVA. The innovative VISX system provides a guide for determining the best refraction for the patient. When there is a difference between the manifest and wavefront refractions, due to corneal or lenticular abnormalities, the PreVue Lens serves as an excellent means of verifying that the wavefront measurement is optimal for the patient. It also gives the patient and doctor a method to validate the type of result that they may achieve from the wavefront-guided ablation.
|
|
|
|
In the VISX wavefront LASIK trial, all eyes were targeted for
emmetropia. |
|
Analyzing the Data
Our data analysis examines the effectiveness of the VISX WaveScan system in terms of uncorrected visual acuity, refractive stability, predictability or intended versus achieved, higher-order aberrations, and responses to a subjective questionnaire on night vision and glare and contrast sensitivity.
The 6-month data is based on 320 eyes of 173 patients with a mean age of 38 years. The mean preoperative sphere was approximately 3.5D with a range of .8D to 6.5D. The mean cylinder was .6D with a range of 0 to 3D. And the manifest refractive spherical equivalent was about 3.2D.
Looking at uncorrected visual acuity at 6 months, 96% of patients in the trial achieved UCVA of 20/20 or better. Moreover, 74% were 20/16 or better and 19% were 20/12.5 or better. And 70% of the treated eyes had the same or better postoperative UCVA compared with their preoperative BSCVA. This is a particularly significant result because in order to qualify for this study, patients had to see at least three letters on the 20/16 line with the PreVue lens.
In terms of key effectiveness criteria, the FDA requires that a minimum of 85% of patients have post-op visual acuity of 20/40 or better; 100% of patients in the VISX trial are 20/40 or better at 6 months. Moreover, 50% of the patients have to be within .5D of the targeted manifest refractive spherical equivalent and 75% within 1D; 95% of patients in the trial were within .5D at 6 months, and 100% were within 1D.
Results have been very stable, with 98% of the eyes having less than a .5D change. In fact, at 3 to 6 months, 99% of eyes had less than or equal to 1D of change. And 100% of the patients were within 1D of intended versus achieved correction at 6 months, and 95% of the patients were within .5D of emmetropia.
|
|
|
|
Post-op, 70% of eyes had UCVA the same or better than their pre-op
BSCVA. |
Comparing patients in the trial who received wavefront-guided treatments with a similar cohort of patients who had conventional treatment, the wavefront group had less of an increase in the higher-order changes. In fact, the majority of custom ablation patients showed an improvement in higher-order terms at 6 months: 78% showed some improvement in coma; 84% showed some improvement in trefoil, and 70% showed some improvement in spherical aberration.
Other Key Findings
In response to a subjective questionnaire, patients in the study were more satisfied with their vision postoperatively in terms of night vision, glare and frequency of halos. In terms of contrast sensitivity, there was no significant difference between the preoperative result versus the postoperative results at 6 months.
As far as BSCVA, 8% of the custom ablation patients gained one to two lines; 58% gained up to a line; 28% had no change; and 6% of the patients lost up to a line, but no patients lost more than three letters of BSCVA.
Two eyes in the group experienced an epithelial defect at the last visit. One patient had 20/12 uncorrected visual acuity and another had 20/16. Three eyes experienced DLK. All three eyes had uncorrected visual acuity of 20/16 at 1 month and were treated with conventional methods. One eye experienced a partial flap, but did not receive laser treatment.
The FDA requires that laser refractive surgery clinical studies have below 5% of eyes with a loss of more than 2 lines of BCVA, below 5% increase of more than 2D or cylinder, and below 1% adverse events. In this clinical study, zero eyes experienced any of these problems: therefore, we can conclude that this is a very safe procedure.
|
|
|
|
At 6 months, patients reported that they were more satisfied with their night vision post-op than with their night vision
pre-op. |
|
Solid Results By Several Measures
In summary, 96% of the eyes treated with the VISX WaveScan system achieved UCVA of 20/20 or better; 74% were 20/16 or better; 70% of the eyes had the same or better postoperative UCVA compared with their preoperative best-spectacle-corrected vision; 95% of the eyes were within .5D of our target; 70% of the eyes had a decrease or less than a 1-micron change in RMS; and no eyes lost a line of their best-spectacle-corrected preoperative visual acuity.
Wavefront-guided LASIK with the VISX WaveScan has proven extremely safe, with virtually no potential for operator error. Based on these results, this platform, which includes the innovative PreVue Lens system, is clearly on track to become the system of choice for performing custom ablations.
Colman Kraff, M.D. is director of the Kraff Eye Institute in Chicago.
THE CARL ZEISS MEDITEC PLATFORM
Enhancing Surgeon Control
over Customization
BY DAN Z. REINSTEIN, M.D., M.A. (CANTAB), F.R.C.S.C.
The philosophy underlying the Carl Zeiss Meditec custom ablation platform is to provide a system of individually optimized components, seamlessly integrated to readily serve the general refractive surgeon, while still affording comprehensive sophisticated control options for the expert specialist.
Preoperative patient clinical data, including ocular aberrometry and corneal shape are integrated and processed by a central software control station, the CRS-Master. The CRS-Master then generates an individually optimized custom ablation profile, specifically designed to enable the MEL80 excimer laser to perform corneal reshaping.
Features of the Technology Suite
The main components of the platform are:
WASCA aberrometer. The Carl Zeiss Meditec WASCA (WAverfront Supported Customized Ablation) device is produced jointly with Wavefront Sciences Inc., who market the same device as the Complete Ophthalmic Analysis System (COAS) in the United States. The WASCA unit possesses the highest lenslet resolution available: 210µm, nearly twice that of the closest competitor.
Such a high resolution directly translates to improved accuracy and reproducibility. This very fine-pitch lenslet array also has an extremely short focal length in order to provide a very large dynamic range (6 diopters). In addition, a patented system forces a focused spot to 'drop out' before it can cross over to the detector field of the adjacent lenslet; therefore, spot-crossing, nominally one of the disadvantages of Shack-Hartman aberrometers, can't occur with the WASCA aberrometer.
MEL80 excimer laser. This laser was designed specifically from the ground up to meet the demands of customized ablation. It operates with a distinct Gaussian beam profile by means of a passive stabilization system (patented), with a 0.8-mm effective ablation spot size at a shot frequency of 250 Hz and a proprietary nonrandom shot-distribution pattern based on thermography studies to minimize cumulative surface heating. The shot frequency affords a considerably foreshortened ablation time; a 5.00D 6-mm zone spherical ablation takes only 15 seconds. Myopic treatments may be performed up to an 8-mm fully corrected ablation zone. The corneal ablation range extends to the 10-mm zone, to ensure optimization of hyperopic and other blend zones.
|
|
|
|
The WASCA aberrometer from Carl Zeiss Meditec. |
|
The infrared active video tracking system, with automatic thresholding and automatic centration, samples at 250 Hz, and the physical delay time for the total system is 2 to 3 ms, which corresponds to the highest standard of tracking performance available today.
Topography. The extended range of the original Meditec TOSCA functions will be included in the CRS-Master, incorporating all the commercially available (except in the U.S.) algorithms already implemented for the MEL70 for the correction of decentrations and small optical zone enlargement.
Moreover, the corneal surface data will be used to compute, according to beam angular dependence, the laser energy adjustment required to deliver a constant fluence to the corneal surface. This will ensure that the delivery of excimer laser pulses is optimized for achieving accurate shape changes on the stromal surface.
CRS-Master. If the human cornea had an average thickness of 900 µm, any patient would be able to safely have his refractive error, wavefront, and asphericity optimized within corneal thickness safety limits. In reality, the human cornea has a mean thickness of 515 µm with 95% of it lying between 440 and 590 µm. (Reinstein DZ, Silverman RH, Rondeau MJ, Coleman DJ. Epithelial and corneal thickness measurements by high-frequency ultrasound digital signal processing. Ophthalmology 1994;101(1):140-6.)
|
|
|
|
The MEL80 excimer laser from Carl Zeiss
Meditec. |
Therefore, based on the individual optical errors and corneal thickness constraints of each patient, certain compromises will need to be made on the degree of prolateness, or the flattening of the wavefront. Compromises in surgery require clinical judgment. Clinical judgment is the function of surgeons. Therefore, the CRS-Master was developed to integrate a sophisticated, theoretical optical application with clinical judgment, effectively allowing surgeons into the loop of ablation profile design.
Given specific desired outcome variables (e.g., optimization for night vision or tissue-saving algorithms), preset buttons enable the surgeon to instantly review suggested profiles. The CRS-Master possesses a module designed to reduce the induction of spherical aberration called ASAP (aberration smart ablation profiling). ASAP was first presented at the ESCRS in Amsterdam 2001. Based on a knowledge of epithelial, biomechanical and laser fluence dynamics, ASAP determines the ideal correction factors required to reduce the induction of aberrations. As not all eyes will be suitable for maximum optimization, one of the future features of ASAP will be the prolate optimization function (POF), which will enable the surgeon to optimize the amount of asphericity delivered in the ablation profile. The CRS-Master custom mode incorporates the WASCA wavefront data into the desired ablation profile, and enables the expert surgeon to personally design the optimum distinct ablation profile for a specific eye. Ablation profile design is assisted by 3-D maps that allow the surgeon to visualize each step of the optimization process.
Preliminary Results
Preliminary results of LASIK performed using the MEL80 incorporating the ASAP module of the CRS-Master (and excluding higher-order wavefront aberration data) were reported by Reinstein and Srivannaboon at the Fourth International Congress on Wavefront Sensing and Aberration-Free Refractive Correction in San Francisco in February of this year. A prospective evaluation of 60 consecutive eyes with a spherical equivalent mean (SD) of 4.51 (ranging from 1.50D to 9.38D) was carried out with 6 months follow-up. All patients were fully evaluated by an independent observer.
Accuracy analysis at 6 months showed a mean postoperative spherical equivalent of 0.05D, with 90% of eyes within 0.25D, and 100% within 0.5D of intended. The predictability (described by the standard deviation of the mean spherical equivalent) at 5 months was 0.18D. Efficacy analysis reflected this level of accuracy and predictability, with 100% of eyes seeing 20/32 or better, 97% seeing 20/25 or better, and 92% seeing 20/20 or better.
Such an optimized nonwavefront-guided system, we believe, forms a substantial platform for the overlay of the high-quality wavefront data provided by the WASCA aberrometer. Studies to integrate all components are underway and results will be reported this year.
Corneal Sculpting at a New Level
The Carl Zeiss Meditec platform for custom ablation incorporates a suite of technology for wavefront aberrometry, corneal surface shape data, highly developed excimer laser delivery, and surgeon-controlled individualization of treatment protocol. Together, these components promise to deliver increasingly higher accuracy and control over corneal sculpting -- a dream to come true for the father of keratomileusis, the late Jose Ignacio Barraquer.
Dr. Reinstein is Medical Director of the London Vision Clinic, London, U.K. He holds several academic positions, including Assistant Clinical Professor at the Weill Medical College of Cornell University. He is the lead surgeon in the development team for the MEL80 excimer laser and CRS-Master.