What's New for Your Practice from the ASCRS Annual Meeting
Wavefront-Guided Treatment of Hyperopia
VISX announced that it will launch its automated iris registration technology for LASIK procedures at the American Academy of Ophthalmology meeting later this year, and that the name of its newly FDA-approved custom ablation platform is CustomVue.
In addition, W. Bruce Jackson, M.D., reported the study team results that led to the international commercial release of hyperopic CustomVue treatments. Bilateral wavefront-guided procedures utilizing the STAR S4 laser with ActiveTrak were performed on 16 eyes of 8 patients (3 men and 5 women with a mean age of 50.9 ±6.5 years) with hyperopia and astigmatism up to +3.0D spherical equivalent. All eyes were targeted for emmetropia, and no nomogram adjustments were made. Optical zones were blended out to a 9-mm total ablation area.
|
|
|
|
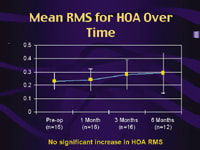
In the VISX study of
wavefront-guided
treatment of hyperopia,
no significant increase in higher-order-aberration RMS was seen. |
Results at 6 months included:
- A no eye lost more than two lines of best-spectacle-corrected visual acuity
- A 100% of eyes achieved 20/25 uncorrected visual acuity; 69% achieved 20/20; and 38% achieved 20/16
- A 94% of eyes were within ±0.50D of target refraction
- A 94% of eyes experienced less than a 0.5D refractive change from 3 to 6 months
- A trends went toward a decrease in spherical aberration and no significant increase in higher-order aberration RMS.
- Dr. Jackson has begun enrollment of a new cohort of patients with up to +6D of sphere and +5D of cylinder.
The Importance of the Peripheral Ablation
Jack Holladay, M.D., M.S.E.E., F.A.C.S., clinical professor of ophthalmology at Baylor College of Medicine in Houston, Texas, discussed a growing concern in LASIK: Most laser platforms don't account for the change in energy being delivered by the beam as it moves toward the periphery of the ablation zone.
Because the cornea is curved, the energy of the beam spreads out more as it moves away from the center of the cornea. According to Dr. Holladay, tissue ablation may be reduced to less than 80% of the amount intended at the periphery. This, he said, is the primary factor causing an increase in spherical aberration of the cornea following LASIK and PRK, as well as producing an oblate corneal shape.
Dr. Holladay said that correcting this problem could cause a dramatic improvement in LASIK results -- much greater than that produced by using wavefront technology to correct higher-order aberrations. In fact, Dr. Holladay said, we won't really be able to determine the benefits of custom ablations until this problem is corrected.
Three laser platforms address this issue: the Carl Zeiss Meditec system, the Lumenis Allegretto laser system, and LaserSight's CustomEyes custom corneal ablation program. International results with the Allegretto, reported at a separate gathering, supported Dr. Holladay's conclusion.
The result of correcting this problem, he added, is an ablation profile that's accurate all the way to the periphery. "Every patient who has had, or will have, excimer laser treatment is affected by this mistake, and all future patients would benefit from correcting it," he concluded.
Microkeratomes and Custom Ablation
Brian S. Boxer Wachler, M.D., speaking at a scientific symposium sponsored by Moria, discussed microkeratome factors that are especially significant for achieving precise refractive outcomes, particularly with custom ablation. He emphasized three key microkeratome characteristics:
Predictability. A microkeratome should have a low standard deviation so that you can be sure of consistently preserving at least 250 microns of posterior stromal bed.
The right flap characteristics. He recommends:
- creating a 110- to 130-micron flap because anterior stroma is smoother than deeper stroma. (The smoother the bed, the less distortion is likely to be induced.)
- a 9.0 to 10.0-mm flap diameter, which can accommodate the typical custom ablation blend zone out to 9 mm.
Flexibility. A nasal hinge may be preferable for dry eye patients because of nerve plexus conservation, but a superior hinge reduces the risk of flap slippage that may be encountered with a nasal hinge.
Dr. Boxer Wachler said he uses Moria's M2 microkeratome, for several reasons: it's automated; it allows him to customize flap diameter based on K-readings; it has a strong dual drive motor; it's easy for his technician to assemble and clean; it's reliable; and it produces thinner flaps. (Preliminary data from Dr. Boxer Wachler's evaluation of flaps produced by the 90 head show a mean thickness of 132 microns ±14 microns [n = 16].)
Dr. Boxer Wachler also recommended that surgeons develop a keratome nomogram to increase predictability. This involves measuring the mean and standard deviation of your keratome to improve the accuracy of your residual stromal bed calculations. (For more on this, see below.)
Microkeratome Labeling vs. Depth of Cut
Several speakers delivered presentations at an AMO event, including CEO James Mazzo, Randall Olson, M.D. (on Sovereign with WhiteStar technology), and Samuel Masket, M.D. (on OptiEdge IOL design).
Kerry Solomon, M.D., director of the Magill Laser Center at the Medical University of South Carolina, and professor at the Storm Eye Institute, presented the results of a study, which indicate that while today's microkeratomes cut consistently, they can cut much thicker or thinner than what they're labeled to cut. "Surgeons can't assume, for example, that a microkeratome labeled 130 will cut a 130-micron-deep flap," he said.
Dr. Solomon and 18 other surgeons across the country recently studied 1,600 eyes and all of the major microkeratome brands with three main goals: to develop standardized labeling, to define thicker and thinner limits for each device with a 95% confidence interval, and to isolate the variables that affect flap thickness. "Standard deviations and mean flap thicknesses were very, very different among the devices," he said.
Most microkeratomes are labeled based on mean thickness or by the thicker limit of the flaps they cut. "So, you might know based on the labeling how thick a device will cut, and that's important because if you cut too thick, you could cause ectasia," Dr. Solomon said. "But you wouldn't know how thin it might cut, which means you could get some buttonhole flaps. Rather than mean thickness, it's more important for surgeons to know how thick and thin a device cuts so they can plan their procedures accordingly."
Beyond this study, Dr. Solomon said, the only way surgeons will know the thickness and thinness of the flaps they're cutting is by measuring them with ultrasonic pachymetry. The surgeons at his facility use a subtraction method of measurement. They take a quick corneal measurement just before the pass with the keratome. Then they lift the flap and take another measurement, dry on the bed.
They note the measurement in the chart, which is helpful for getting comfortable with what their keratomes are cutting, and being able to switch to another head or another keratome when necessary in a certain case. Also, "I may have planned my surgery for a 180-micron flap, but I know what my flap thickness really measures, so I know whether I have room to enhance or not," Dr. Solomon said.
Also among the study findings:
- The two least variable devices were AMO's Amadeus 140 and Nidek's MK-2000 145. The Amadeus 140 had a mean thickness of 134, with a standard deviation of 15.5 microns. "If we follow that out to a 95% confidence interval, it's going to cut between 103 microns and 165 microns 95% of the time," Dr. Solomon said.
The Nidek 145 had a mean thickness of 103 microns, with a standard deviation of 14.5. It had a 95% confidence level at 74 microns to 132 microns. - Several factors correlated with flap thickness, including mean pre-op pachymetry. Thicker corneas tended to have thicker flaps, and thinner corneas tended to have thinner flaps.
- The flaps of second eyes tended to cut 10% thinner than first eyes.
This type of information is even more important when it comes to custom ablation because "We tend to use more tissue," Dr. Solomon said.
|
|
|
|
The subepithelial separator, invented by Ioannis
Pallikaris, M.D., creates a flap
for surface ablation without
using alcohol. |
|
New Keratome and Epithelial Separator
CIBA Vision Corporation will market and distribute BioVision AG's Centurion SES microkeratome in the United States and most other countries. The device, which has 510(k) approval, has a proprietary cutting system that integrates the blade and cartridge into one component. It also uses a bar applanator, rather than a plate applanator, to flatten the cornea. The bar design applanates only the section of the cornea directly in front of the blade, resulting in a feathered cut and smoother-edged, "gutterless" flaps.
Later this year, CIBA Vision plans to introduce the Centurion SES separator, which will mechanically create epithelial flaps for surface ablation procedures. Among the surgeons speaking at the Charles D. Kelman Innovator's lecture was Ioannis Pallikaris, M.D., Ph.D., inventor of the device. The SES pushes the top layer of the epithelium out of the way mechanically, thus avoiding the use of alcohol, which Dr. Pallikaris believes may damage the epithelial flap.
It uses a blunt blade and low suction to mechanically separate a hinged epithelial flap. A dry, custom contact lens is placed over the flap; the flap sticks to the lens, making it easy to lift and flip over nasally. After laser ablation the flap, together with the contact lens, is placed back on the eye. This procedure has been named epi-LASIK.
Advantages of the new procedure include:
- The flap separates below the basement membrane. (When alcohol is used, the cleavage plane falls within the basement membrane.) Dr. Pallikaris says that leaving the membrane intact provides much more stability and support for the epithelium. Electron microscopy has confirmed that the basement membrane is preserved.
- Using the SES and contact lens minimizes flap manipulation.
- Unlike a LASIK microkeratome, the separator doesn't cut into the stroma. As a result, accidental loss of the flap isn't the kind of major problem it can be in LASIK.
- Early trials have shown that patients have high-quality vision by the first day post-op.
The Pros and Cons of the IntraLase FS
|
|
|
|
|
Jeremy Meltzer, M.D., discussed the rate of complications he's experienced when working with -- and the advantages of -- LASIK flaps made with the IntraLase FS laser.
Dr. Meltzer said that problems with DLK after use of the IntraLase have been overstated. Out of 1,000 cases performed using the IntraLase, only 46 complications developed, including 15 cases of DLK (1.5% of patients), 11 flaps that needed repositioning, and 8 cases of abrasion.
"The IntraLase is a technological improvement over the microkeratome, but it's not perfect," Dr. Meltzer observed. "It causes inflammation a little more often, but when the instrument's settings are correct, it's a relatively minor problem." (He explained that the only time the settings need adjustment is after the technician recalibrates the laser.)
Dr. Meltzer listed numerous advantages he's experienced using this technology:
- He's able to make thin flaps safely, so more patients are candidates for the procedure.
- The Intralase flap has caused noticeably fewer complaints about dry eye after the surgery. Dr. Meltzer reported that his practice was nearly removed from a multicenter study of a dry eye medication because almost none of his post-LASIK patients qualified for the study.
- Unlike a microkeratome, Dr. Meltzer said that a break in suction when making a flap with the IntraLase isn't a big problem; you can simply reapply the suction ring and pick up where you left off.
- The hinge can be placed anywhere.
- Dr. Meltzer's outcomes have been equal to or better than his outcomes with microkeratome flaps -- without the flap complications. He hasn't had to deal with any free or mangled caps, buttonhole flaps or incomplete flaps.
- Using the IntraLase has resulted in less post-op follow-up and handholding.
- Because you can directly observe the flap location and use software to direct the pattern before starting, flaps are optimally centered every time.
- Keratome flaps tend to be meniscus-shaped, whereas IntraLase flaps have a consistent depth across the entire flap. This may be significant in terms of inducing fewer higher-order aberrations from flap creation.
Dr. Meltzer added that he found the IntraLase procedure easy to learn, and believes other surgeons will have the same experience.
LASIK vs. LASEK: Flaps and Aberrations
Scott MacRae, M.D., professor of ophthalmology and visual science at the University of Rochester in New York, presented results of a study designed to test the hypothesis that customized LASEK might induce fewer higher-order aberrations than standard LASIK because no flap is created during LASEK. This seemed a reasonable possibility because of two groups of previous studies: One group showed that custom PRK or LASEK lowered the amount of higher-order aberration; the other demonstrated that a LASIK flap can induce a 30% increase in some higher-order aberrations.
Dr. MacRae's study involved 19 patients. One eye received custom LASEK; the other received conventional LASIK. Both procedures used identical ablation zones. Results indicated no significant difference between the procedures in induced higher-order aberration. However, at 3 months, customized LASEK eyes had a smaller increase in spherical aberration (58%) than the conventional LASIK eyes (94%). These findings suggest that there may be some advantage to surface ablation with regard to spherical aberration, but further studies seem warranted.
Dr. MacRae also wanted to compare results from customized LASIK and LASEK. However, FDA regulations prevented him from performing customized LASIK in the first study, so he made further comparisons using data from a separate study in which he performed customized LASIK on 340 eyes using the Bausch & Lomb Zyoptix ablation system, with a follow-up of 6 months.
A comparison of these outcomes with those following customized LASEK showed that:
- Acuity results were excellent after either procedure.
- Custom LASIK using Zyoptix does reduce higher-order aberration, especially if the eye has at least 0.5 microns RMS of higher-order aberration before the procedure. (Dr. MacRae noted that a larger group of customized LASEK eyes will need to be treated to confirm this same observation with customized LASEK.)
Confocal Microscopy and LASIK
At this year's Charles D. Kelman Innovator's lecture, a number of surgeons discussed their latest work. Herbert E. Kaufman, M.D., board professor of ophthalmology, pharmacology and microbiology at the Louisiana State College of Medicine in Baton Rouge, talked about the advantages of using confocal microscopy, particularly in relation to LASIK.
Dr. Kaufman described confocal microscopy's ability to reveal what lies inside tissue as being much like tomography; it makes it possible to observe a specific cross-section, or layer, of the tissue. As examples, Dr. Kaufman said he has observed debris left behind by microkeratome blades that were reused; he's been able to see fungus clearly enough to identify the type; and he's seen amoebae and infectious agents, signaling the need for immediate treatment.
Confocal microscopy is also a valuable tool for evaluating epithelium recovery after LASIK. Dr. Kaufman said he's able to accurately judge the extent of stromal hydration, and evaluate how treatment is affecting tissue below the surface, making it much easier to know when treatment is complete and medication can be stopped. "You can see things deep in tissue that can't be tested for in any other way," he concluded.
Given the compact and accurate nature of today's confocal microscopy instruments, Dr. Kaufman said he expects this technology to become a significant part of most practices.
|
|
|
|
Calvin Roberts, M.D., presented the results of his study, which indicated that pre-op dosing with the NSAID Acular reduced pain for cataract surgery patients. |
Controlling Cataract Surgery Pain
It is known that nonsteroidal anti-inflammatory drugs (NSAIDs) decrease pain for refractive surgery patients. Now, evidence has been presented that shows the same holds true for cataract surgery patients.
"Anesthesia is critical to topical clear cornea cataract surgery because we are replacing traditional injection anesthetics with just drops," said Calvin Roberts, M.D. He performed a study in which 296 patients were randomly assigned to either receive 3 days of ketorolac (Acular) q.i.d. prior to cataract surgery or receive no preoperative NSAIDs. All patients were anesthetized with 2% xylocaine jelly, and received ketorolac drops on the day of surgery along with their dilating drops. On the first post-op day, the patients completed a questionnaire.
"We found that the patients who had 3 days of pre-op Acular had a statistically significant decrease in discomfort associated with their surgery than those who did not take pre-op Acular," Dr. Roberts said. "By prescribing Acular, and the soon-to-be-available reformulation, I know I'm using a formulation that is comfortable and safe for my patients."
In Other News
► Stephen Slade, M.D., F.A.C.S., presented results from the FDA clinical trial of the Bausch & Lomb Technolas 217A laser for treating hyperopia. The trial was conducted at eight sites throughout the United States. Results were tabulated after 358 eyes (bilateral procedures) were treated for both sphere and cylinder with no nomogram adjustment. Mean patient age was 53.1 years; mean sphere and cylinder were 1.92D and 0.5D respectively.
At 6 months post-op:
- 61.4% achieved 20/20 uncorrected visual acuity or better and 94.8% achieved 20/40 UCVA or better
- 81.4% maintained or improved night-driving vision
- 98.9% reported overall improvement in their quality of vision; the majority indicated marked improvement
- 74.1% of patients maintained or improved their best-corrected visual acuity.
Dr. Slade said that after 9 months, 98% of patients achieved refractive stability within 1D of the intended result. Studies of Zyoptix treatments of hyperopia have begun, with more than 40 eyes enrolled to date.
► Biosyntrx has launched a 10-site clinical trial of BioTears Oral GelCaps, its patent-pending systemic treatment for dry eye syndrome. The gelcaps were formulated around the most recent research in lipid metabolism and target the inflammation associated with dry eye. According to Biosyntrx president Spencer Thornton, M.D., the study is addressing the standard clinical markers found in the dry eye patient and will provide important clinical information for professional peer-review, which has not been traditionally available on indication-specific nutraceuticals.
► Refractec Inc. reported that it sold 30 Viewpoint CK systems during this year's meeting, generating $1.5 million. Since FDA approval of conductive keratoplasty to correct hyperopia in April of last year, more than 10,000 procedures have been performed. CK is now being studied as a treatment for presbyopia.
► ScienceBased Health has added MacularProtect Complete to its macular health product line. "MacularProtect Complete provides three critical benefits for high-risk patients," said Penny Edwards, M.P.H., C.N.S., nutrition scientist for ScienceBased Health. "It provides the antioxidants that are clinically proven to preserve vision and macular health; it incorporates meaningful amounts of lutein and zeaxanthin, two carotenoids essential for macular health; and it provides a full spectrum of the vitamins, minerals and plant compounds important for preserving overall health."
Ron P. Gallemore, M.D., Ph.D., a partner in the Retina-Vitreous Associates Medical Group in Los Angeles, and an assistant clinical professor at UCLA's Jules Stein Eye Institute, said that many patients have trouble taking supplements in addition to a multivitamin. "MacularProtect Complete contains it all and should simplify supplementation, improving compliance, safety and efficacy," he said.
► Volk Optical introduced the Digital 1.0x lens for general diagnostics and slit lamp imaging and photography. The lens provides a 60° static field of view and a 72° dynamic field of view of the posterior pole. Like all Volk lenses, the Digital 1.0x is double-aspheric. Anti-reflective coating and a unique glass design help to reduce glare and reflections.
|
|
|
See the May issue of Ophthalmology Management or visit www.ophthalmologymanagement.com for more news from the meeting. |