Ramping Up for Custom
Ablation
Part Two: Figuring out the financial impact.
(See
Part One)
BY DESIREE IFFT, EXECUTIVE EDITOR
The LASIK business at the Montreal practice of Gordon Balazsi, M.D., is better than it's been for quite some time. Procedure volume is up. One of his television ads, on the shelf since last year, is back on the air. Soon, he'll be hiring five new staff members and increasing his fee -- for the second time since the bottom fell out of the market.
Poor night vision had become one of the most feared complications. But with custom, "I know that night vision has improved in a high percentage of patients," Dr. Balazsi says. "On subjective questionnaires, a third of our patients tell us their night vision is improved compared to pre-op. Although we can't prove it, this has probably helped to restore confidence in the procedure. The quality of vision we're getting with custom is better than with standard. Also, our percentage of 20/16s and 20/12s is higher than with standard. Sixty percent of our eyes gain one line or more of BCVA; with standard that number was around 30%. Contrast sensitivity improves in the vast majority of patients, especially in dim light.
"We've never seen this before in refractive surgery. These results allow us to charge a much more reasonable fee," more in line with costs and a worthwhile profit margin.
Can Custom Turn Things Around?
Historically, what has happened in the Canadian LASIK market has happened in the United States about a year and a half later. Does that mean U.S. LASIK has a recovery on the way? Industry watchers expect a small bump in case volume this year. Medical laser expert Irving Arons predicts 15% growth, primarily due to wavefront-guided procedures. "I believe that some 1,437,500 procedures will be done in 2003, up from the 1,250,000 likely done in 2002," he's said. Consultant John Pinto predicts "no more than a 10 to 20% lift in most markets in terms of leads and cases."

However, practices that have begun to formulate financial plans for custom aren't necessarily counting on an increase in volume. Instead, they expect to be able to recoup their costs by charging a premium fee, up to $500 more per eye than they're charging for standard LASIK. (See "Working with the Numbers," on page 81.) Scott Hyver, M.D., for example, who practices in the competitive San Francisco Bay area, is transitioning to custom based on these numbers:
How Many Patients Will We Treat?
Dr. Hyver considers his estimate that 20% of his LASIK patients will undergo a custom procedure a conservative one. It doesn't take into account new patients who might be drawn into the field of LASIK because of the arrival of custom, he says. The numbers other practices anticipate are anywhere from 10 to 50%. Dr. Balazsi says that in a given week, 60 to 80% of his LASIK patients undergo a custom procedure. (In Canada, on the B&L system, he's able to treat up to 12D of myopia with custom.) Louis Probst, M.D., a TLC-affiliated surgeon in Canada and the U.S., reports that 30% of his LASIK cases in Canada are custom.

At this point, practices have somewhat different ideas about which patients they'll want to have a custom procedure. "It is not clear at this point," says Dr. Probst, "that all patients who fit the FDA criteria will benefit from custom LASIK. Studies have shown that patients who have less than 0.4 microns of higher-order RMS aberrations preoperatively don't really seem to benefit from custom."
According to Dr. Hyver, "One of the things that's really important to us in this practice is that even though custom is going to come out with a lot of hype, for some patients to pay this premium price for LASIK is going to be overkill. A lot of patients -- with normal pupils, basic prescriptions, and a low degree of higher-order aberrations -- are still great candidates for traditional LASIK." He will strongly recommend custom for patients with significant pre-op higher-order aberrations. He will explain to the others that both standard and custom are good solutions and let them choose.
Mitchell Jackson, M.D., Chicago, is waiting for his Alcon custom equipment package to be delivered. Once he's up and running, he'll perform custom on all patients who fit the FDA criteria (also subject, of course, to the usual constraints such as eye health and tissue availability). "If they qualify for a wavefront-guided treatment and have a low or high pre-op RMS, why should I do a conventional treatment and increase their higher-order aberrations? Most studies have shown that's what we do with standard LASIK. Why put patients at increased risk of that?"
Michael Lawless, M.D., of New South Wales, Australia, agrees. "We're doing custom to reduce pre-op higher-order aberrations, but also to induce fewer. I don't think you can not offer it to everybody who qualifies." That said, he notes, "We wrestled with how to place this in the market without confusing new patients and causing concern to patients who didn't get this technology. So, we say this is an improvement, but there have been lots of improvements over the years, and this is just one of them. We don't go into a lot of detail on custom vs. standard. If a patient is suitable under the FDA guidelines, they get custom. If not, they get standard."
Avoiding Past Mistakes
The positioning of custom LASIK is definitely something to think about. As Terrence O'Brien, M.D., Baltimore, said during a recent seminar, "How we communicate 'custom' will make all the difference between success and failure. Doctors need to rebuild patient confidence in the safety of LASIK."
Consultant Shareef Mahdavi offers similar advice. He says practices should focus on the patient, not the technology: "Forget about the my-laser-is-better-than-your-laser approach. Honest communication and quality customer service are what's needed." He also recommends that the message focus on safety, not efficacy. "Don't hype 'supervision,' " he warns. "The real potential of custom LASIK lies in the ability of wavefront to screen patients more effectively, thereby reducing the number of '20/20 unhappies.' " Dr. Probst tells his patients that he believes custom LASIK is their best chance of getting quality vision. "But I also tell them that it's certainly not a 100% chance," he says. "That's an important distinction because if patients are looking at custom LASIK as perfect now, we may be creating some very unrealistic expectations. What we're really dealing with now is the first edition of what will be at least a ten-edition evolution of wavefront."
If Not Now, When?
Still, he and other practices that believe in the technology are choosing to make the transition as soon as possible. As Ralph Hyver, head of marketing at ScottHyver Visioncare puts it: "If you're not in the custom LASIK business, are you really in the LASIK business at all?

CUSTOM
CORNEA FROM ALCON
Focusing on Quality of Vision
BY OMAR HAKIM, M.D.
Improving the quantity of vision used to be the main goal of custom ablation. Clinicians were focused on traditional measures, such as the percentage of patients achieving a certain level of uncorrected visual acuity or best-corrected visual acuity (BCVA).
While quantity of vision is still crucial, clinicians are now placing more emphasis on quality of vision. Newer measures of visual quality include contrast sensitivity, low-contrast visual acuity, and assessment of higher-order aberrations. Given custom LASIK's ability to reduce or eliminate induced aberrations, it is a procedure clinicians should offer to every patient who fits within the approved treatment range.
When we're performing custom procedures, we have to deal with three major technical requirements:
- measuring the wavefront
- treating the wavefront
- registration.
In this article, I'll discuss these three areas in more detail, in the context of the Alcon CustomCornea System.
Measuring the Wavefront
While measuring higher orders of aberration may be important in virgin eyes, it becomes crucial with highly aberrated eyes, such as symptomatic post-LASIK eyes. The LADARWave allows measurement of up to eighth-order aberrations.
This Hartmann-Shack-based, second-generation aberrometer can measure from -14 to +8 diopters with up to 6 diopters of astigmatism. It measures up to 210 points over a 7-mm pupil. It also features automatic fogging, which controls accommodation, and an optimized lenslet array design that allows measurement of higher-order aberrations by reducing crossover effects. The device also provides a large instantaneous dynamic range. It can measure points on the eye that are vastly different in terms of aberration without the use of compensation lenses.
|
|


|
|
|
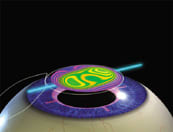
Alcon's "Capture-Match-Treat" registration process is
engineered to ensure that the custom ablation profile is in exactly the same relationship to the eye as the measured
wavefront. A registered treatment is shown top and bottom left. A misaligned treatment is shown top and bottom
right. |
|
|
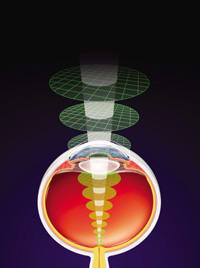
Treating the Wavefront
As you know, a complex ablation requires removing small amounts of corneal tissue. The LADARVision laser provides a 0.8-mm ablation spot. With a Gaussian beam profile, the LADARVision can ablate up to 60 spots/second. The Gaussian beam provides a much smoother ablation than a "top-hat" beam.
Also of benefit is the nonsequential fashion in which the device places the pulses. This avoids a local thermal effect, which ensures that each ablative pulse has a predictable result, by allowing the relaxation of the tissue from the previous pulse before a new pulse is applied to the same area of the cornea.
Uniquely, the LADARVision uses an active, closed-loop laser radar eye tracking system, consisting of a series of four diode lasers aimed at the pupil margin. Energy from the diode lasers is reflected back to the device at 4,000 times/second. This provides minimal lag time, as the eye can move only 1/4000 of a second before the tracking system recognizes the movement and repositions the laser.
Registration
The process of registration links the ablation to the wavefront. With the Alcon platform, this process is referred to as the "Capture-Match-Treat" registration process. This process ensures that the custom ablation profile is in exactly the same relationship to the eye as the measured wavefront. Specifically, with the Alcon system, you use a corneal surgical marking pen to place two ink marks at the limbus at approximately the 3 and 9 o'clock positions. Then you dilate the pupil and place the patient in front of the LADARWave.
You then place a reference line through those two ink landmarks. This, in combination with a limbal ring, fixes the eye. You can now measure the wavefront and create an ablation profile.
Now, you take the patient to the laser. You place the limbal ring in exactly the same position. The eye tracker ensures that the eye is locked in an x-y orientation. Then you place the same horizontal reference line through those two limbal ink marks. By doing this you have compensated for cyclotorsion of the eye. This ensures that the eye is in the same position as when the wavefront was measured.
This "Capture-Match-Treat" process ensures that the ablation profile will be in the correct position when you do the treatment. This is crucial because, even with a perfect wavefront, if you don't place the ablation in the same position as when you measured the wavefront, you could induce more aberration than the eye had previously.
Even misregistration of the ablation of as small as a quarter millimeter or cyclotorsional effects of less than 5 degrees will give you a worse result. In essence, you'll have worsened the problem -- performing a conventional treatment would likely have provided better results.
This is especially important in post-surgical eyes with large amounts of aberration. Many of these eyes have a limited amount of residual corneal tissue to work with, and you may not be able to perform further surgery to correct problems created as a result of misregistration.
Improving Vision Quality
As we are learning, both creating the flap and its healing can affect the biomechanics of the cornea. But this response is predictable to an extent. You can get a better final result by taking these flap-induced biomechanical and healing effects into consideration when you convert the wavefront into an ablation profile.
The Alcon system applies these predictable biomechanical effects to the wavefront to obtain a better result. Using the proprietary CustomCornea algorithm, the wavefront provides an ablation profile that aims to leave the flattest postoperative wavefront possible.
The results obtained with the Alcon system are promising. For instance, in the CustomCornea Study Group, principal investigator Stephen Brint, M.D., found impressive results in uncorrected visual acuity at 3 months. In fact, after 3 months, 100% of all eyes (n = 36) and spherical eyes (n = 15) reached 20/25 or better; 75% of all eyes and 87% of spherical eyes reached 20/16 or better.
Significant gains also occurred in BCVA after 3 months. Preoperatively, only 6% had 20/12.5 or better (n = 36); at 3 months, 33% had reached that mark (n = 36). Some 97% of eyes had BCVA of 20/16 or better at 3 months postoperatively compared with 86% preoperatively.
Besides these results, custom ablation provides a significant improvement in spherical aberration compared with conventional treatment. Conventional treatment increased spherical aberration by 136% over preoperative levels at 6 months postoperatively (n = 138). In contrast, with custom ablation, at 6 months postop, spherical aberration increased by only 11% (n = 422). This is a dramatic reduction in the induction of postoperative spherical aberration. With the latest refined CustomCornea algorithm, at 3 months the increase in spherical aberration was virtually nonexistent at 1% (n = 143).
This research also demonstrated that on average, total higher-order aberration and coma induction declined with custom ablation procedures compared with conventional treatment. The declines were in the range of 50%.
The CustomCornea Study Group found that the benefit of the lower higher-order aberrations after wavefront-guided surgery corresponded to approximately 0.2 diopters of defocus error.
Finally, contrast sensitivity under mesopic conditions at 6 months showed an improvement in eyes after wavefront surgery. Some 18% experienced a significant increase in contrast sensitivity, versus a decline in 8% of eyes. A significant change was defined as a change of greater than 0.3 log (more than two levels) at two or more spatial frequencies.
Many Patients Can Benefit
These findings reinforce the argument that all patients can benefit from custom ablation. Not only may we want to eliminate pre-existing aberrations, selectively, but we want to minimize the induction of further aberrations. The evolution of this process should ultimately result in better quality vision for patients.
Dr. Hakim is Medical Director, TLC Laser Eye Centers in London, Waterloo, and Toronto, Ontario, Canada. A Fellow of the Royal College of Surgeons of Canada, he serves as a Principal Clinical Investigator in the CustomCornea Study Group, conducting FDA studies of CustomCornea. He was the first surgeon outside the United States to perform this surgery.
NAVEX FROM NIDEK
New Algorithm Looks Promising
BY MIHAI POP, M.D.
The NAVEX custom ablation system consists of three main technical components:
|
|
|
|
One hundred
percent of 314 NAVEX treatments reported by Dr. Mihai Pop were within +1D (green lines) of the intended target. Preoperative sphere ranged up to 8.25D, and cylinder ranged up to 3D. |
|
OPD-Scan. The OPD scan is a combination aberrometer and topographer. It uses the principle of spatial dynamic skiascopy to measure the aberrations of the eye and placido disk topography to measure the corneal shape. The measuring principle consists of a projecting system, which is an infrared light-emitting diode housed within a chopper wheel with slit apertures.
The receiving system consists of a photodetector array that converts the time differences of stimulation into dioptric power maps. The dioptric power maps, or refractive maps, are displayed as "OPD maps," from which traditional Zernike-based maps out to the eighth order can be derived. In contrast to traditional Hartmann-Shack and Tscherning-type aberrometers, the OPD exploits time differences of stimulation rather than positional differences to map the aberrations of the eye. This difference in measuring principles allows the measurement of highly aberrated eyes and eyes with large refractive gradients. Additionally, it has a comparatively wide measuring range of 20D to +22D of sphere and up to 12D of cylinder. An added benefit is that aberrometry and topography are performed on the same instrument, so axis of alignment is not an issue with this wavefront platform.
Final Fit software. This software uses both topography and aberrometry to develop the ablation algorithms.
EC-5000 CX excimer laser. The laser employs both scanning slit and spot ablation capabilities to deliver the treatment onto the cornea. The beam is Gaussian and has a spot size of 1 mm. The optical zone can be varied to 6.50 mm, and the transition zone can be varied out to 10 mm.
NAVEX allows the treatment of primary refractive surgery candidates in addition to the treatment of patients who have had suboptimal outcomes from previous refractive surgery. A newly available cyclotorsion module, which is based on iris details, allows compensation for cyclotorsion that may occur between the sitting (OPD) to supine positions (EC-5000 CX).
|
|
|
|
One-month post-op results from a series of 314 NAVEX treatments
(216 available for follow-up) on myopic and astigmatic patients as reported by Dr. Mihai Pop. |
Clinical Outcomes
We recently completed NAVEX LASIK treatment for myopia and astigmatism on 314 virgin eyes. Preoperative sphere ranged up to 8.25D, and cylinder ranged up to 3D. These patients are a representative sample from a refractive surgery center and were not preselected for a certain level of visual acuity prior to wavefront correction.
All treatments were based entirely on OPD-Scan measurement and the Final Fit ablation plan, without nomogram adjustment. This automated approach reduces the risk of human error. One hundred percent of the treatments were within +1D of the intended target, yielding highly accurate and reproducible results. Eighty six percent of the patients were within +0.50D of the intended target. At 1 month post-op, among the 126 patients available for follow-up, 90% achieved 20/20 or better uncorrected visual acuity, and 48% achieved at least 20/15 uncorrected visual acuity.
The automated approach was safe. None of the eyes lost best-corrected visual acuity, and 92% of the eyes had UCVA within one line of the BCVA. Fifty four percent of the patients gained at least one line of best-corrected visual acuity. Both eyes of one patient were undercorrected. He was re-treated with NAVEX, and his BCVA was maintained 1 month postoperatively.
|
|
|
|
A small effective optical zone following a conventional ablation for a 5D correction is signified by the red ring on instantaneous topography. (Image courtesy of Paolo Vinciguerra M.D.) |
|
Higher-order root mean square (RMS) increased postoperatively by only 0.083 microns (1.4x). Data for a representative sample of the NAVEX-treated patients for individual higher-order aberrations such as coma and trefoil show that approximately half of the patients experienced decreased RMS values postoperatively. Subjectively, patients expressed a very high degree of satisfaction with NAVEX treatments.
These results support the safety and accuracy of the treatment of myopia and astigmatism by NAVEX. Postoperatively patients have excellent unaided visual acuity.
Future Developments: Customized Aspherical Transition Zones
Various excimer laser manufacturers have reported large increases in spherical aberration after excimer ablation. This higher-order aberration has been implicated in a variety of night vision disturbances along with a generalized decrease in BCVA.
Recently NIDEK introduced an ablation algorithm that specifically addresses the issue of spherical aberration. Essentially this involves increasing the transition zone, reducing the optical zone and creating a seamless transition between the optical and transition zones and nascent cornea.
Preliminary results from Paolo Vinciguerra M.D., and Arturo Chayet, M.D., on human eyes did in fact confirm that there is a reduction in the amount of induced spherical aberration. The advantages of this unique treatment method are that it actually decreases ablation volume, creates a prolate cornea, and increases the effective optical zone. By moving what Vinciguerra refers to as the "red-ring" on corneal topography past the pupillary excursion diameter and reducing the severity of contour change, the spherical aberration that would normally affect the point spread function is effectively reduced. (See images, above.) The red ring on instantaneous (or tangential) topography often has a deep red ring after laser ablation. The severity of the color signifies abrupt dioptric power changes in the cornea between the optical zone, transition zone and nascent cornea. The diameter of the ring signifies the effective optical zone.
|
|
|
|
A large effective optical zone after creation of a NAVEX customized aspherical transition zone for a 6.00D -1.5D X 90 correction is signified by the red ring on instantaneous topography. (Image courtesy of Paolo Vinciguerra
M.D.) |
By introducing patented ablation algorithms in the treatment zones, the NAVEX platform reduces these abrupt dioptric power changes and consequently the spherical aberration induced by many conventional excimer lasers. The prolate nature of the cornea postoperatively has the added advantage that the coupling of aberrations between lens and cornea is not disrupted to the same extent as with a conventional ablation, which induces oblate cornea. The use of the OPD-Scan and Final Fit software allows the simulation of the postoperative aberrometry and topography maps. The customization of the effective optical zone to a specific pupil size is also possible within the Final Fit software.
A number of investigative sites have produced encouraging initial results, such as maintenance or increases in contrast sensitivity and subjective quality of vision. The advent of this unique ablation algorithm allows refractive surgeons to taper treatments that maintain quality of vision in photopic and scotopic conditions.
Dr Pop, a world-renown refractive surgeon, is the Director of Cliniques Michel Pop in Montreal and Hull, Canada. He is currently conducting clinical trials with Nidek.
THE VISUAL FUNCTION ANALYZER FROM TRACEY
The Role of Ray Tracing Technology
BY DAVID R. HARDTEN, M.D.
With the advent of custom refractive surgery, it has become increasingly important to understand the physics of vision. Longstanding diagnostic instrumentation such as corneal topography has enabled today's refractive surgeons to more greatly appreciate the detail and variability of the cornea's shape and hence its refractive power. With the cornea providing roughly 70% of the refractive power of the eye, it is a critical element, but not the entire picture. We need an exact understanding of a patient's optical system to achieve optimum visual results with our treatments.
New instrumentation has now been introduced into the LASIK procedure that needs to be understood to properly optimize the techniques for analysis of the optical system. Currently, most manufacturers utilize Hartmann-Shack technology and principles to generate their data on higher- and lower-order aberrations to guide wavefront-assisted ablations. The Hartmann-Shack system uses a lenslet array, which measures aberrations of the eye from a single point on the retina (fovea) in a reverse fashion out the exit pupil.
|
|
|
|
Comparison of refractive maps and higher-order aberrations in two eyes seeing 20/20 uncorrected following conductive keratoplasty 2 years ago. The patient with no complaints has less than 1/3 the amount of higher-order aberrations as measured by root mean square
(RMS) values and has smaller pupils in dim illumination than the patient complaining of
halos. |
|
Measuring Highly Aberrated Eyes
Our visual system, though, has forward aberrations, that is, a light source from outside of the eye is focused by the visual system and imaged on the retina. Ray tracing, or LASEREFRACTION, technology from the Tracey Visual Function Analyzer (Tracey-VFA) measures forward aberrations by determining the retinal location of a light ray projected into the eye. With Hartmann-Shack devices, the lenslet array measures all points within the pupil simultaneously and is therefore susceptible to data confusion by highly aberrated eyes. The Tracey-VFA's LASEREFRACTION measures each point of light sequentially, minimizing confusion from the crossing of data points.
Recently, VISX announced a Letter of Intent agreement with Tracey Technologies to work toward incorporating the Tracey-VFA into the VISX wavefront-guided ablation system. We have had the Tracey-VFA system for more than a year and have found it uniquely useful for evaluating those patients with a large amount of higher-order aberrations, who are patients that would theoretically benefit the most from a wavefront-guided ablation. In our practice we have been able to measure and follow our most aberrated corneas: keratoconus patients, patients post-penetrating keratoplasty, pellucid marginal degeneration and severely decentered excimer laser ablations.
|
|
|
|
Refractive maps with progressively larger pupils in a patient complaining of glare in dim illumination following implantation of an iris-supported phakic
IOL. An area of abnormal reflective surface is seen superiorly as the pupil enlarges past 4.5 mm. The higher-order aberrations also increase significantly as the pupil enlarges. |
The Tracey-VFA is able to measure highly aberrated eyes because of its method of acquiring data. It directs as many as 95 separate and temporally sequential points of light in five concentric arrays into the entrance pupil within 1/8 of a second. Since each point of light is sequential, much like bullets coming out of a Gatling gun, the detection device has no problem differentiating one point from another. This allows the Tracey-VFA to easily measure a large dynamic range of aberrations and maintain high-resolution detail of each sampled point.
With aberrometers that project all points of light simultaneously, there is the chance of data confusion by points of light crossing over another point, where it is not possible to determine the relationship of the points. The location of each point of light that is directed into the eye is detected by the Tracey-VFA. This provides a true "point spread function" of vision outlining the image a patient has projected on the macula ("ray tracing"). This image results from measuring forward aberrations, which are in the same direction that the patient visualizes the images.
The Tracey-VFA's observation and focusing system allows it to measure pupils from 2 mm to 8mm depending on the patient. Preliminary studies have demonstrated that for eyes imaged on both Hartmann-Shack and the Tracey devices the data is very similar. This suggests that the Tracey-VFA when linked to the laser has the potential to accurately direct treatment for standard custom ablation algorithms as well as difficult irregular corneas.
Pinpointing Patient Symptoms
While the use of the Tracey-VFA for deriving wavefront aberrations is certainly exciting and promising, on a day-to-day basis we rely on it as an extremely helpful diagnostic tool. The device not only allows us to understand the visual effects of refractive surgery and other pathologic processes, but when patients present with visual symptoms for which we have no ready explanation, it frequently pinpoints the problem allowing us to demonstrate to the patient that we understand what is causing their difficulty.
A good example of the phenomenon comes to mind. Recently we had two patients present to our office 2 years post-conductive keratoplasty. Both were seeing 20/20 uncorrected; however, one patient was extremely happy and the other complained of halos around lights in one eye. Evaluation with the Tracey-VFA showed that the eye with the halos had 3 times the amount of higher-order aberrations as the other 20/20 eye. (See image below.)
|
|
|
|
Refractive maps from two patients following
LASIK. The patient on the left had a 6-mm ablation zone, and the presence of spherical aberration is obvious by the ring of yellow/red in the periphery indicating an area of more myopic refractive error. On the right is a more recent 8-mm ablation zone with virtually no spherical aberration. Total higher-order aberrations are 4 to 5 times more in the 6-mm ablation
case. |
|
We have also had the opportunity to follow some IOL patients (cataract and refractive phakic) who have noted glare in certain lighting. We have been able to document abnormal reflective surfaces in some of them and the presence of lens edge glare in others. (See image, above right.)
The Tracey-VFA can also be used to monitor changes in LASIK techniques that have improved outcomes. Recently we were part of a study performing 8-mm optical zone ablations and have seen dramatic decreases in induced spherical aberration when compared with our earlier 6.5-mm ablation zones. (See image at right.)
Adding the Power of Topography
Tracey is adding a new dimension to measuring higher- and lower-order aberrations by adding the input from the EyeSys handheld topography unit, the Vista. Using the EyeSys topography data, the Tracey instrument can separate out the aberrations caused by the anterior cornea from those present in the crystalline lens or the posterior cornea.
We've found the Tracey-VFA to be robust and accurate, and it has proven to be an invaluable diagnostic tool. It appears that it also has potential to be a major input device for custom ablation systems.
Dr. Hardten is Director of Refractive Surgery at Minnesota Eye Consultants in Minneapolis and a Clinical Associate Professor of Ophthalmology at the University of Minnesota.