Clinical News: MEDICAL AND PRODUCT UPDATES
Transciliary Filtration -- Without Bleeding
Although procedures such as trabeculectomy have helped to save the sight of many glaucoma patients over the years, relieving pressure through the cornea has many drawbacks -- drawbacks that could be eliminated if the filtering pore were made through the sclera instead. But until recently, creating a channel through the sclera into the ciliary body usually caused excessive ciliary bleeding, an unacceptable side-effect in all but the most extreme cases.
Now, the unique technology of the plasma blade (also known as the Fugo Blade, after its inventor, Richard Fugo, M.D., Ph.D.) is making it possible to perform transciliary filtration without triggering ciliary bleeding. The new procedure, called "Singh filtration" after it's inventor, Daljit Singh, M.D., of Amitsar, India, also eliminates many of the problems inherent in trabeculectomy.
|
Why Doesn't the Wound Bleed? |
|
|
Unlike a conventional blade, the plasma blade creates an incision by ablating tissue much in the same way a laser does. (In fact, both use photons to disrupt molecular bonds between molecules.) Apparently, the plasma field surrounding the tip creates microparticles as it breaks apart molecular bonds. The microparticles plug the capillaries, and at the same time stimulate platelet activity and trigger coagulation. (However, as Dr. Fugo has noted, a really big vessel incised by the plasma blade might need cautery.) The plasma blade doesn't cauterize tissue; it leaves a clean margin, with no collateral tissue damage. Surgeons performing the procedure have begun referring to this blood vessel-sealing phenomenon as "autostasis," making Singh filtration an "autostatic" procedure. |
|
|
|
Steps in the procedure
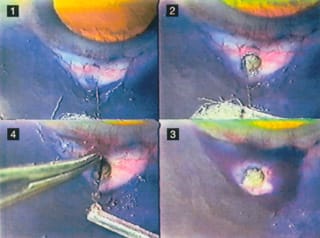
To perform Singh filtration using the plasma blade:
Check the condition of the lymphatics. The lymphatics will have to carry away the fluid released through the new channel. This is easily accomplished by injecting a bleb of a vital stain such as trypan blue and making sure the fluid is moving through the lymphatic system.
Make a 1-cm conjunctival flap. The flap could easily be made using the plasma blade, but for now researchers are using scissors so that if a complication occurs its cause can be isolated.
If any bleeding is observed at the scleral surface -- a much less significant problem than ciliary bleeding -- it's important to avoid extensive cautery. Using minimal, pinpoint cautery will avoid damaging the lymphatics of the eye, which would undermine the benefits of the surgery.
Create a pit in the sclera. Once the flap is pulled back, the plasma blade, fitted with an extra-thick tip, is used to create a 1.0- to 1.5-mm round pit in the sclera, down to the ciliary body. (You can tell when you've reached the ciliary body because the tissue is a different color.) The pit is placed pre-Tenons in order to avoid Tenon cysts, which can lead to an uncontrolled increase in eye pressure.
Make a micropore. Once the pit is created, the surgeon uses the plasma blade, fitted with a thin tip, to make a micropore through the ciliary body. When the channel is deep enough, fluid begins to seep out (as opposed to gushing out). This is important, because pressure in the eye falls slowly, with no shallowing of the anterior chamber.
Replace the flap. Once a satisfactory "ooze" is observed, the flap is replaced and sutured with a single suture.
|
|
Profiling the Plasma Blade |
|
|
The plasma blade is a lightweight, portable, handheld device that generates a cloud of plasma particles around a tiny filament (about as thick as a human hair) at the end of the handpiece. The plasma particles dissolve the molecular bonds of the material they come in contact with, creating an incredibly sharp, resistance-free incision. The incision is 20 to 40 times sharper than an incision made with a diamond blade, and in most surgical conditions produces minimal or no bleeding. The unit is powered by two AA-sized rechargeable batteries, which power the blade for about an hour on a single charge. The FDA has already approved the plasma blade for use in capsulotomy. (For a description of the advantages of this technique, see "Plasma Capsulotomy" in the August, 2001 issue of Ophthalmology Management.) |
|
|
Advantages of transciliary filtration
In comparison to trabeculectomy, which can take 30 to 45 minutes to perform and is associated with flat anterior chambers, choroidal effusion, unpredictable post-op pressure and hyphema, Singh filtration has numerous advantages:
- it only takes 5 minutes to perform
- it causes minimal trauma
- it has fewer side effects
- surgery can be revised quickly and easily
- it requires less post-op care
- it poses less risk to the patient.
Because the pore is placed behind the iris, this procedure is effective even in cases of angle closure.
Clinical data
Currently, more than 250 eyes, including a large percentage with severe pathology, are enrolled in human clinical trials. So far, results have shown:
- IOPs have been stabilized at acceptable levels
- no flat anterior chambers resulted from the surgery
- no hyphema occurred
- 11 surgical revisions were required, but the surgeons reported that the revisions were technically simple and took little time
- two choroidal effusions were reported, but they were resolved with conservative management.
For further information
More information on the Fugo Blade and these procedures is available at www.fugoblade.com, or by contacting Dawn Michelle DelCampo, president of Medisurg Research and Management Corporation, at 100 West Fornance St., Norristown, Pa. 19401.
|
|
|
1) Trypan blue has been injected under the conjunctiva to reveal the integrity of the lymphatics, and a 1-cm fornix base flap has been raised along the limbus. 2) A 1.5-mm pit has been ablated into the sclera; a hair-thin plasma blade filament extends from the bottom center of the photo into the pit. 3) The ablation filament has placed a 120-micron pore through the ciliary body into the pre-hyaloid space behind the iris. Aqueous is slowly oozing from the pore. 4) Aqueous flow through the micropore washes a drop of trypan blue away from the scleral pit. The conjunctival flap is ready to be repositioned along with limbus with a single suture. |
|
One-Minute Filtration |
|
Offshore surgeons are also testing a variation on Singh filtration that takes 1 minute to perform. In this variation, the surgeon raises a small bleb with lidocaine. Then conjunctival tissue is pulled a little to the side with forceps so that the conjunctiva overlying the targeted scleral position is displaced a few millimeters from its normal location. The plasma blade is used to place a 150-micron filtration track through both conjunctiva and sclera, in either the pre-iris area or the pars plana. At the end of the procedure, the bleb is pushed back to its natural anatomic location so the conjunctival perforation is at a reasonable distance from the intraocular perforation. The success rate at 2 months post-op shows viable filtration blebs in 70% of patients. This number is anticipated to increase as the technique is further refined. (Two patients out of 50 demonstrated choroidal effusion, which resolved over the course of 10 days.) |








