Patient Management
BIOPTICS:
More than the Sum of its Parts
With this combination procedure, surgeons have achieved
dramatic results in patients with high refractive errors.
By Jonathan M. Davidorf, M.D.
Bioptics -- the technique that combines phakic IOL and LASIK -- may not yet be available in the U.S., but outside this country it's found a place in correcting extreme refractive errors. The procedure is gaining a foothold wherever surgeons are implanting phakic IOLs. I believe we'll see bioptics performed here on a widespread basis shortly after the FDA approves the first phakic IOL.
For patients with high refractive errors, the one-two punch that bioptics provides can offer dramatic improvements in vision. Using the two procedures in tandem gives results that neither procedure can achieve alone for extreme refractive errors.
Working in Argentina, Roberto Zaldivar, M.D., first conceived bioptics and was the first to perform the planned two-staged procedure in 1996. In this article, I'll offer a detailed look at bioptics, including a step-by-step review of the surgical procedure. First, let's define the term.
Working in two planes
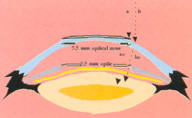
The term bioptics was coined because the optical correction is split between two planes: the ciliary sulcus plane (IOL) and the corneal plane (LASIK). The procedure offers two important theoretical advantages:
- It maximizes the final effective optical zone size because the optical zone size of each procedure is maximized.
- It improves the predictability of results. That's because the patient's subjective refraction during the LASIK portion of the procedure is more reliable given the overall reduction in myopia after phakic IOL insertion.
|
|
|
|
In bioptics, once the phakic IOL is implanted, the LASIK procedure doesn't have to correct an extreme refractive error. Therefore, when the procedures are combined, it's possible to correct a -20D eye, for example, with an effective optical zone of at least 5.5 mm. With LASIK or phakic IOL alone, the effective optical zone would be much smaller, increasing the risk of visual aberrations. |
|
Patient selection
The typical bioptics patient has spherical myopia of more than 15D or compound myopic astigmatism of 12D or greater. This compares with LASIK, which is most suitable for patients with a refractive error up to 10 or 12D spherical equivalent. It also compares with phakic IOL implantation alone, where patients with essentially spherical myopia do well up to 15 to 19D, depending on the phakic IOL model.
In a study conducted by myself, Dr. Zaldivar and others, patients with up to 35D spherical equivalent refraction were treated. (See "Study Results at a Glance".)
Contraindications for bioptics are generally similar to those for other elective refractive procedures. Conditions that rule out bioptics include cataracts, corneal degeneration, diabetic retinopathy, dry eye, glaucoma, keratoconus, retinal tears, and previous IOL surgery. Additionally, the anterior chamber must be at least 3 mm deep to allow for proper placement of the phakic IOL.
IOL specifics
In performing the phakic IOL portion of bioptics surgery, most of my experience is with the STAAR Collamer posterior chamber phakic IOL. To avoid postoperative pupillary block, I recommend two laser iridotomies superiorly at least 60 degrees apart to avoid simultaneous obstruction of both iridotomies by the IOL's plate haptic. Some surgeons advocate surgical iridotomies at the time of IOL implantation, although this is somewhat more invasive and may increase pigment dispersion.
The patient can be sedated either with oral medication or via infusion, similar to cataract surgery. The eye is dilated, prepped, and draped as it would be for cataract surgery.
Topical anesthesia or a peribulbar block may be used. Using a peribulbar block in long myopic eyes requires special caution to avoid penetrating the globe with the peribulbar needle.
A superior and inferior paracentesis are made followed by the injection of a cohesive viscoelastic. Using less than a 3-mm blade, a clear corneal incision is fashioned temporally.
The implantation of the STAAR Collamer IOL for bioptics is similar to a post-cataract implantation. Because the lens sits on top of the eye's crystalline lens, some vaulting must occur between the crystalline lens and the phakic IOL. Special caution is needed when positioning the haptics to avoid contact with the crystalline lens. These surgical manipulations are somewhat more critical in crowded hyperopic eyes.
I insert diluted Miostat, which gives a more sustained response than Miochol. Using a low-viscosity, cohesive viscoelastic facilitates viscoelastic removal with a standard irrigation/aspiration system after IOL implantation. The wound edges are hydrated, not sutured.
As with cataract surgery, patients receive post-op antibiotic and steroid drops. Some surgeons use oral Diamox, and some place the patient on topical ocular antihypertensives.
The refraction is usually stable in a week, but it's prudent to wait at least 4 weeks before performing LASIK. This ensures the stability of the refraction and security of the incision.
|
|
Study Results at a Glance |
|
In a study conducted by myself, Dr. Zaldivar and others (J Refract Surg 1999; 15:299-308), 67 eyes underwent bioptics. Preoperatively:
Postoperatively:
|
On to LASIK
Because of the phakic IOL insertion, the LASIK procedure doesn't have to correct an extreme refractive error. It's possible to correct a 20D eye, for instance, with an effective optical zone of at least 5.5 mm by combining the two procedures. (See image on previous page.) Using LASIK or phakic IOL alone, the effective optical zone would be much smaller. The larger optical zone lessens the risk of visual distortion or, as my colleague Amar Agarwal, M.D., calls it, "aberropia."
One alternative to this series of steps involves making a flap before inserting the phakic IOL, as suggested by Jose Guell, M.D., when using the Artisan lens from Ophtec. When the patient's vision stabilizes following phakic IOL implantation, the surgeon lifts the flap, as with a standard LASIK enhancement, and performs the laser ablation. Surface ablation as opposed to LASIK may also be employed.
Big gains
We've found incredible gains in best-corrected vision using bioptics. With phakic IOL alone, more than a third of patients may be expected to gain two or more lines of best-corrected vision when treating high myopia. But with bioptics eyes, which typically have even higher refractive errors, more than three-quarters of patients may gain two or more lines.
In our previously mentioned study, 69% of bioptics eyes achieved 20/40 or better uncorrected visual acuity postoperatively, while only 30% of eyes saw this well with spectacles before surgery. These results almost begin to look like those for cataract surgery.
More than the sum
While the FDA considers bioptics experimental, the procedure has found a place in correcting the most extreme refractive errors. Results may well improve along with advances in phakic IOLs, lasers, and microkeratomes.
In a sense, with bioptics, the whole is greater than the sum of its parts.
Dr. Davidorf is medical director of the Davidorf Eye Group in West Hills, Calif., and clinical instructor of ophthalmology at the Jules Stein Eye Institute in Los Angeles.