Glaucoma Case Studies
Case One
Is this glaucoma or not?
Patient history/examination: An 11-year-old African-American male was referred for evaluation. He had a history of myopia and on routine eye examination was found to have elevated intraocular pressure (upper 20s OU). Past medical history included attention deficit disorder for which he was taking no medication. Family history was unknown because he was adopted. He had no known drug allergies. He was taking generic timolol 0.25% in each eye twice daily, and Xalatan 0.005% in each eye in the evening. He was tolerating the medication without side effects.
His visual acuity was 20/25 in the right eye with a refraction of -3.75 + 0.25 X 130, and 20/30 in the left eye with a refraction of -5.00 + 1.00 X 110. His color vision was normal in each eye. The pupils were equally round and reactive to light with no afferent pupillary defect. Extraocular movements were full, with a small exophoria at near.
|
|
|
|
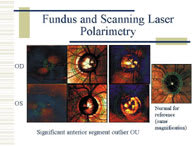
Fundus image of each eye taken from the GDx scanning laser
polarimeter. |
|
The slit lamp examination was normal with no iris transillumination defects or endothelial spindles. The anterior chamber angle was open to the ciliary body, with 2+ pigmentation of the posterior trabecular meshwork. The lenses were clear. Intraocular pressure (on medication) measured 17 mm Hg in the right eye and 22 mm Hg in the left.
The fundus exam showed very large discs in each eye (megalopapilla), with a cup-to-disc ratio of 0.8 to 0.9 in each eye. The vessels, macula, and nerve fiber layer looked normal in each eye. Scanning laser polarimetry was performed to assess the retinal nerve fiber layer. (See "Fundus and Scanning Laser Polarimetry," above, left.)
Visual fields were performed twice. (See "Visual Fields, FASTPAC Strategy," below.) Both times, the visual field testing was unreliable and uninterpretable because of the patient's attention deficit disorder. The scanning laser polarimetry data was not conclusive due to anterior segment compensation issues and megalopapilla (insufficient nerve fiber layer data in residual image).
|
|
|
|
Visual field results for each eye, performed twice (8 days apart). FP = false positives; FN = false negatives. |
Discussion: Is this a case of glaucoma? The initial elevated intraocular pressure readings and the large cups in each eye would suggest that it is. However, the optic nerve images, scanning laser polarimetry, and visual fields are compromised by artifact and poor performance. The cup-to-disc ratio is increased in each eye due to large discs, so even the optic nerve appearance cannot be used conclusively. There are no congenital anterior segment abnormalities to suggest juvenile glaucoma. So, the remaining question is whether the baseline (untreated) intraocular pressure readings are correct.
Artifact, such as squeezing of the eyelids or a narrow palpebral fissure (with the lid riding on the tonometer during pressure measurement), may give rise to falsely elevated pressure readings. Neither was present in this case. The other major influence on intraocular pressure reading with the Goldmann applanation tonometer is central corneal thickness. Because the instrument assumes a central corneal thickness of approximately 535 microns, if a cornea is significantly thicker, it takes more force to applanate it. Therefore, a false high pressure reading will be obtained. (The opposite is also true; thinner corneas underestimate the pressure.)
In this case, the central corneal thickness as measured with an ultrasonic pachymeter was 613 microns in each eye. Therefore, the intraocular pressure was overestimated by 5 to 7 mm Hg OU, depending on the algorithm used. Certainly the intraocular pressure on medication corrects to 10 to 18 mm Hg in each eye, which is normal.
Continued management: Despite evidence to the contrary, this could still be glaucoma. The intraocular pressure is currently in normal range with no side effects from medication. Therefore, it was elected to continue treatment for the time being with the recommendation that visual field testing be carried out every 6 months until reliable information can be obtained.
Case One was submitted by Neil T. Choplin, M.D., who is a glaucoma specialist with Eye Care of San Diego and an adjunct clinical professor of surgery with Uniformed Services University of Health Sciences in Bethesda, Md.
If you would like to comment on this case, e-mail Ophthalmology Management at ifftda@boucher1.com.
Case Two
Challenges beyond the clinical
Patient history/examination: The patient is a 40-year-old mentally handicapped woman. Gonioscopy showed her to have occludable angles in both eyes (anterior chamber angles with a grade I approach based on Schaffer's classification) and to be at risk for developing bilateral acute angle-closure glaucoma. She is a +2 hyperope. The patient's legal guardian refuses any laser or surgical treatment for the patient.
The patient's intraocular pressure hovers in the mid-teens, and her cup-to-disc ratios are 0.5 OU. There is no evidence of pseudoexofoliaton. An ultrasound demonstrated no mass lesion. The patient is unable to perform visual field testing.
Discussion: This case represents some of the social challenges we face as we try to convey the importance of preventing a serious ocular emergency and provide the standard of care for a condition. In difficult cases, a court order may be necessary to enable us to proceed with any laser or surgical treatment.
For this patient, I prescribed pilocarpine 1% b.i.d OU and explained all potential side effects to the guardian. Close monitoring is necessary because pilocarpine can have one of two mechanisms of action. It can widen the anterior chamber angle, or it can move the lens-iris diaphram forward, increasing the risk of acute angle-closure glaucoma. Therefore, gonioscopy was performed again 1 week after the first instillation.
It was also important to inform the guardian of the high risk of blindness from an acute angle-closure attack. The guardian was also advised to avoid any over-the-counter medications, such as Benadryl, which can increase the risk of acute angle-closure glaucoma.
Continued management: The patient's status at this point is guarded. Follow-up is scheduled for every 3 months. OM
Case Two was submitted by Mary A. Bhavsar, M.D., a glaucoma specialist with Eye Care Associates, P.A., in Minnesota.
If you would like to comment on this case, e-mail Ophthalmology Management at ifftda@boucher1.com.