Retina Surgery
on the Move
Advances in instrumentation fuel
the trend toward ASC procedures.
By Eddie F. Kadrmas, M.D., Ph.D.

I have received communications from a number of retinal specialists, from California to Massachusetts and from North Dakota to Florida, expressing their desire to set up their own retina ASCs. Many of them have done so. Retina surgery in the ASC is certainly alive and well and continues to grow in popularity.
This is due in part to the amazing advancement in surgical technology, which is making procedures safer for our patients, as well as more cost- and time-efficient for us. The following pages provide an overview of what we've been working with in our practice, as well as a list of new tools available to vitreoretinal surgeons.
Patients and surgeons benefit
High-speed vitreous cutters, such as those manufactured by Bausch & Lomb, Alcon and Dutch Ophthalmic Research Center, have decreased vitrectomy times significantly and have, most importantly, made the procedure more precise and safer for the patient. Other companies, too, such as Synergetics, have been developing instrumentation that improves quality of care and convenience for patients, and streamlines procedures and minimizes personnel and overhead costs for surgeons -- all factors that foster the movement toward ASCs.
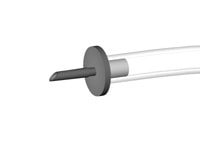
For the past several months, I've had the opportunity to work with B&L's Millennium TSV25 System. This 25-gauge transconjunctival standard vitrectomy system was developed by Eugene de Juan, Jr., M.D., and colleagues at the Microsurgery Advanced Design Laboratory at the Doheny Eye Institute of the University of Southern California. It streamlines procedures by allowing surgeons to operate through a self-sealing microincision. The system thereby eliminates dissection of the conjunctiva and the creation of standard scleral incisions.

Although not all retina surgical procedures lend themselves to the use of this system, it appears to be ideal for some of the more common procedures we perform, such as surgical management of macular puckers, macular holes, vitreomacular traction, some diabetic traction detachments and some simple rhegmatogenous detachments. It may also be ideal for some of the newer procedures, such as radial optic neurotomy for central retinal vein occlusion and arteriovenous sheathotomy for branch retinal vein occlusion. It's useful in some pediatric cases, too, because the small instrumentation is ideal for small eyes.
In cases that require larger instrumentation than will fit through the 25-gauge cannulas, I've still been able to use the TSV25 system, by performing a limited peritomy and enlarging a sclerotomy. Although this requires closure of the tissues, I find that it does not make the case significantly less efficient.
Assessing the limitations
As with any new technology, however, there is a learning curve, and instrumentation and techniques need to be designed and refined. Current instrumentation is somewhat limited for the TSV25 system. For example, as of this writing, Bausch & Lomb has not released an endolaser probe for clinical use. As of late October, however, a laser probe is available from Synergetics, in addition to an endoilluminator and other instruments for 25-gauge use.
Recently, I spoke with Michael Trese, M.D., of the Associated Retinal Surgeons in Royal Oak, Mich. Dr. Trese has extensive experience with the TSV25 system, and he feels that although the 25-gauge high-speed cutter is faster than a traditional 20-gauge cutter, the smaller lumen of the instrument requires the system to run on relatively high aspiration. This slows the cutter down compared with its 20-gauge counterpart.
Also, the smaller port tends to get clogged when he's performing a vitrectomy with admixed hemorrhage. Dr. Trese feels that enzymatic vitreolysis will solve this problem and also play an important role in future vitreous surgery, especially when used with a 25-gauge system. He has used autologous plasmin enzyme for this purpose and has found it to work well. He is currently devising a kit for general use by retina specialists. Dr. Trese says that vitrectomy with the use of plasmin in essence becomes more aspiration than cutting. Hyaluronidase is also under study for this purpose.

Dr. Trese believes that the combination of 25-gauge surgery and enzymatic vitreolysis will eventually make it possible for us to perform vitreoretinal surgery in-office. A big obstacle there, he says, are the current regulations governing facility approval and accreditation.
"It will take a major change in the structure of the current system before in-office surgery can be a reality," he says. "Maybe once payers realize the cost savings that can take place, things will change."
In the meantime, retina surgery in an ASC, when it can be done, is clearly the way to go for many surgeons. And further incentive from Medicare and other third-party payers wouldn't hurt that effort either. Based on the progress made so far, retina surgery will follow cataract surgery to the ASC, where patient- and physician-friendly, cost-effective care is at its best.
Eddie F. Kadrmas, M.D., Ph.D., is a vitreoretinal surgeon in private practice in Plymouth and Dartmouth, Mass. He is an Instructor in Ophthalmology at Harvard Medical School and a member of the Editorial Board for Ophthalmology Management. He has no financial interest in any of the products mentioned in this article.
Michael T. Trese, M.D., is a vitreoretinal surgeon with Associated Retina Consultants in Royal Oak, Mich. He is a Clinical Professor of Biomedical Sciences at Oakland University and a Clinical Associate Professor of Ophthalmology at Wayne State University. He has financial interest in the commercial development of autologous plasmin.
|
Updating Your Armamentarium |
||||||||||||
FROM ALCON:
FROM DUTCH OPHTHALMIC USA (a subsidiary of the Dutch Ophthalmic Research Center):
FROM SYNERGETICS:
FROM VOLK OPTICAL:
|