Rx Perspective
Why I Switched to a Different Anti-Infective
A cataract and refractive surgeon outlines what he sees as the advantages of levofloxacin for prophylaxis.
BY DOUGLAS KATSEV, M.D.
Ophthalmology has indeed benefited from the continued improvement of the fluoroquinolone class of antibiotics. We currently have several effective, well-tolerated options. But bacteria are notoriously resilient, so as surgeons we must be constantly watchful of whether our patients remain protected in the perioperative period.
A growing body of evidence suggests to me that this may not be the case. Some of our most widely used topical fluoroquinolones have been shown to leave a gap in the coverage of Streptococcus, raising doubts about how well they work against gram-positive organisms, which are usually responsible for infectious keratitis after refractive surgery and endophthalmitis after cataract surgery. Furthermore, other studies have shown that with our increased use of larger incisions for the clear cornea technique for cataract surgery has come an increased incidence of endophthalmitis.
|

|
|
|
Source: CORNEA Vol. 20 (3) p301-305 |
|
Also, we shouldn't ignore the issue of resistance. Among the research into this area are the findings of Drs. Busbee and Recchia from Wills Eye Hospital. From July 1989 to July 2000, 248 cataract patients at the facility developed endophthalmitis. From 1989 to 1994, 23% of cultures were resistant to ciprofloxacin (Ciloxan); from 1995 to 2000, 37% of cultures were resistant to ciprofloxacin, a pronounced increase.
WHAT THE RESEARCH TELLS ME
For these and other reasons, I've been using levofloxacin (Quixin) as my fluoroquinolone of choice for cataract and refractive surgery prophylaxis. It has been shown to provide broader coverage against gram-positive organisms than other fluoroquinolones, with no loss of good gram-negative coverage. As far as resistance, Quixin provides the highest concentration of active drug available (0.5%); it rapidly achieves and maintains therapeutic levels of drug in ocular tissues; and it has demonstrated antimicrobial efficacy both in vivo and in vitro.
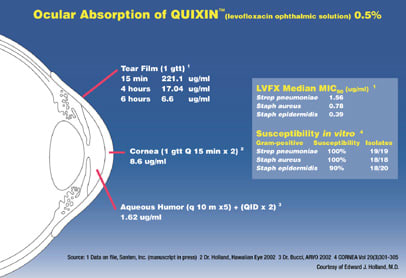
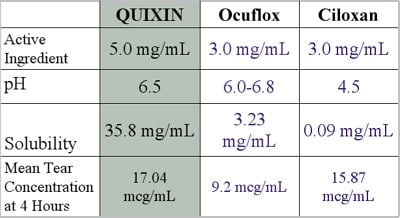
It has excellent ocular absorption properties that are due to its enhanced solubility. Across the pH range, Quixin is the most soluable fluoroquinolone. It exhibited the highest tear film levels at 4 hours based on a single drop, maintaining levels well above the MIC90 of Pseudomonas, Streptococcus and Staphylococcus. And a study by Dr. Bucci presented at this year's ARVO meeting demonstrated that Quixin can achieve therapeutic levels above the MIC90 for both Staphylococcus and Streptococcus in the aqueous humor. This is important, as using a fluoroquinolone on the ocular surface alone does not kill 100% of the flora.
MY SOLUTION FOR TODAY
It probably won't be long until we have access to a fourth generation of topical ophthalmic fluoroquinolones. But until we've worked out exactly how they will fit into our armamentarium, the option that makes the most sense to me for cataract and refractive prophy laxis is Quixin. In addition to the available evidence of its effectiveness, I've been convinced by the decline in surgical complications in my practice since I made the switch.
|
|
|
|
Sources: Solubility and pH data from Physician's Desk Reference for Ophthalmology 2002. Ciloxan solubility data from Ross DL, Riley CM. Aqueous solubilities of some variously substituted quinolone antimicrobiols. Intl J Pharmaceutics. 1990;63:237-250. Tear data from Limberg M. Bugge C. Tear concentrations of topically applied ciprofloxacin. Cornea. 1994;13(6):496-499. |
Dr. Katsev has been in practice in Santa Barbara, Calif., for 12 years.








