Patient Management
Axial Length: DO YOU MEASURE UP?
One surgeon makes the case for changing from
applanation ultrasonography to more accurate alternatives.
By Warren E. Hill, M.D., F.A.C.S.
During the past decade, refractive expectations for cataract surgery have been steadily increasing. Patients have come to view cataract surgery as both a rehabilitative and refractive procedure, and for better or worse, surgeons are now being judged mainly by their refractive outcomes. Gone forever are the days when being within 2 diopters of the intended target was acceptable.
A number of factors can affect the accuracy of your outcomes, including keratometry errors, a capsulorhexis that fails to contain the optic of the IOL within the capsular bag, using outdated IOL power formulas, or IOL constants that haven't been carefully optimized. But measuring axial length correctly is at least as important, and with so many opportunities for error, optimizing every piece of the equation is crucial.
That's why, if you're still using applanation A-scan ultrasonography, I urge you to consider switching to a more accurate alternative. The applanation A-scan technique is an old and trusted friend, but today, any increase in measurement accuracy can make a difference, both to your patients and your practice. Switching from applanation to immersion A-scan ultrasonography or optical coherence biometry (OCB) can significantly increase the accuracy of your IOL power calculations.
|
Using the Prager Shell |
|||||
ultrasound probe a fixed distance from the cornea, surrounded by a small amount of coupling fluid. This coupling fluid can be saline solution, Goniosol, BSS, or artificial tears. With the ultrasound probe maintained at a constant distance above the cornea, and with the patient looking directly at the ultrasound probe fixation light, measurements are very consistent (see charts, next page). A Prager shell can be ordered from Thomas Prager, Ph.D. by calling (281) 389-8776. [Editor's note: Dr. Hill has no financial interest in the Prager shell.] |
|||||
The limits of applanation
The majority of ophthalmology practices today measure the axial length of the eye using applanation (i.e., contact) A-scan ultrasonography. However, most surgeons would probably agree that the applanation technique lacks the accuracy and reproducibility necessary to meet the more demanding requirements of refractive lensectomy and multifocal intraocular lenses.
In today's refractive landscape, applanation A-scan ultrasonography falls short in several areas:
Corneal compression. Applanation A-scan ultrasonography produces a variable amount of corneal compression, anywhere from 0.14 mm to 0.35 mm, which produces a falsely short reading of axial length. Even in the best hands, the amount of corneal compression often changes from one measurement to the next. Also, a fluid meniscus between the probe tip and the cornea can cause a falsely long axial length.
Results are operator-dependent. Usually, the technician with the most experience is most likely to take measurements that are on axis and maintain the same degree of corneal compression. In larger practices it's common to rely on one particular technician who is especially skilled to take these measurements.
Multiple measurements are usually necessary. A common approach is to take a series of readings and then delete those of questionable quality. Measurements are repeated until an acceptable degree of consistency is obtained. (The axial length printouts on page 59 compare the consistency of measurements made by applanation and immersion A-scans; note the variability between the first five measurements made using applanation.)
The advantages of immersion
Surgeons and their staff members often have misconceptions about the mechanics of immersion A-scan ultrasonography. It's perceived as uncomfortable for the patient, time-consuming and technically difficult. In reality:
- It produces less corneal irritation for the patient.
- It takes very little time.
- It's less operator-dependent than applanation.
- When the ultrasound beam is properly aligned with the visual axis and the probe tip is held at a fixed distance above the cornea by the Prager shell, the reproducibility from one measurement to the next is excellent.
Most important, you'll get accurate readings more often using the immersion technique -- and that means better outcomes for your patients. A skilled and experienced ultrasonographer using applanation A-scan ultrasonography will usually produce an outcome within 0.50 diopters of the intended post-operative target refraction about 75% of the time. In comparison, careful use of the immersion technique can increase this number to about 90%. (See graphs, right.)
If you're contemplating entering the arena of refractive lensectomy, transition to the immersion technique is an important first step.
The advantages of OCB
The Zeiss IOLMaster measures the axial length of the eye using partial coherence interferometry, more commonly known as optical coherence biometry (OCB). This new technology has several advantages:
Accuracy. Used properly under normal conditions, the IOLMaster is consistently accurate to within 0.02 mm. When combined with either the Holladay 2 formula, or an IOL- and surgeon-specific optimized version of the Haigis formula, refractive outcomes with the IOLMaster can be astonishingly accurate. (See graphs, right.) The IOLMaster makes it possible to consistently achieve outcomes within 0.25 diopters of the intended target refraction.
However, because the IOLMaster is an optical device, any significant axial opacity, such as a corneal scar, dense posterior subcapsular plaque, darkly brunescent cataract or vitreous hemorrhage will reduce the signal-to-noise ratio to the point that reliable measurements aren't possible. In these cases, A-scan ultrasonography is required. (This occurs in about 10% to 15% of cases.)
The IOLMaster axial length display also provides a signal-to-noise ratio for each reading, telling you whether the ocular media is clear enough for an accurate measurement. Clear ocular media, or mild or moderate lens opacities, yield high signal-to-noise ratios, while dense cataracts show very low signal-to-noise ratios. Measurements showing a proper axial length display can be accepted as accurate even with a signal-to-noise ratio as low as 1.6.
I recommend that 20 axial measurements of each eye be taken. Accuracy is confirmed when at least four of these measurements are within 0.02 mm and the display shows the correct axial length display configuration.
Speed. The IOLMaster measures very quickly. It takes less than 5 minutes to measure both eyes of the average patient in our office.
|
|
|
|
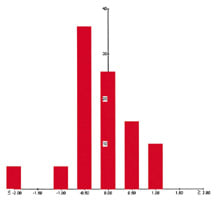
Frequency distribution of spherical equivalent prediction error
(in diopters) by applanation A-scan, immersion A-scan, and
optical coherence biometry. Note that 75% of applanation patients are within 0.50D; 90% of immersion patients are within 0.50D; and 90% of OCB patients are within 0.25D of the intended target
refraction. |
|
Refractive, not anatomic axial length. As long as the patient is able to see well enough to look at the small red fixation light, axial length measurements are made to the fovea. This means that you're actually measuring the refractive axial length, rather than the anatomic axial length.
Unusual eye conditions. The IOLMaster faithfully gives the true axial length as a near routine measurement in eyes with posterior staphyloma, silicone oil, or in the presence of an IOL.
In my opinion, the IOLMaster represents the most significant advance in axial length measurement technology in the past 3 decades.
Updating your constants
When adopting the immersion technique or switching to OCB, you'll need to change your lens constants because these measurements are more accurate. Failure to do so will, on average, result in about +0.50 diopters of unexpected hyperopia.
I recommend that you increase previously optimized applanation IOL constants to prevent postoperative hyperopia. For example, when using the SRK/T formula, A-constants should be increased by 0.50. Similarly, previously optimized Holladay 1 formula Surgeon Factors, and Hoffer Q and Holladay 2 anterior chamber depths (ACD) should be increased by 0.29.
After you've analyzed the postoperative refractive data from the first 10 to 20 cases, you can refine these initial immersion lens constants further.
A change for the better
The level of accuracy we're now being asked to achieve makes OCB and the immersion technique attractive alternatives to applanation A-scan ultrasonography. Still, practices have been slow to change. Switching to immersion A-scan ultrasonography has probably been hindered by force of habit and misconceptions about the difficulty of the immersion technique; switching to OCB has been hindered, at least in part, by the cost of purchasing an IOLMaster.
Nevertheless, the need for greater accuracy in every aspect of IOL surgery is only going to increase. If you're unwilling or unable to invest in an IOLMaster at this point in time, at least consider switching to immersion ultrasonography. Either way, your outcomes should reflect the change for the better.
Note: Additional information on immersion A-scan ultrasonography can be found on the Internet at: www.doctor-hill.com/a-scan.htm. For more information about OCB and the IOLMaster, visit www.humphrey.com.
Warren E. Hill, M.D., F.A.C.S., is medical director of East Valley Ophthalmology in Mesa, Ariz. He specializes in challenging intraocular lens power calculations and unusual anterior segment surgery.
|
|
|
|
Five initial readings made by the applanation technique (above) and immersion technique (below). Note the variability between measurements when using applanation, compared with the consistency when using immersion. |
|