Spotlight:
On Technology And Technique
Correction Without Ablation
For many patients, conductive
keratoplasty may be as effective as LASIK -- and considerably safer. Here's the latest data.
BY CHRISTOPHER KENT,
SENIOR ASSOCIATE EDITOR
For most myopes, LASIK still seems to be the refractive surgery of choice. But LASIK results with hyperopes have been somewhat less impressive. Hyperopic treatment options such as keratoplasty are looking like viable -- perhaps even preferable -- alternatives.
One of the most promising new treatments for mild hyperopia is conductive keratoplasty (CK), which has been in clinical trials in the United States for several years. Clinical data continue to demonstrate the safety and effectiveness of the procedure, which is performed using the ViewPoint CK System from Refractec Inc.
|
|
|
|
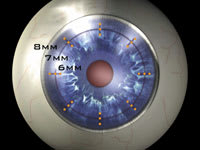
Top: Eight meridians of three circles (one circle marked) tell the
surgeon where the probe should be inserted. Below: The tightened band of tissue causes the desired change in corneal curvature. |
|
How it works
To perform CK, the surgeon inserts a thin probe into the stroma in carefully delineated spots around the peripheral cornea. The number of spots used determines the extent of correction. (See top image, left.) The probe emits radiofrequency energy for 0.6 seconds. Collagen tissue's natural resistance to this energy produces heat, increasing the temperature of the tissue around the probe to 65° C, causing a column of collagen about 150 microns wide and 500 microns deep to shrink. Shrinkage is uniform along the length of the probe.
A series of these columns is placed in a circle around the visual axis; striae form between the columns, creating a band of tightened tissue surrounding the visual axis. This causes a steepening of the central cornea, correcting the pre-existing refractive error. (See bottom image.)
The procedure is performed under topical anesthesia, using one of the lid speculums that come with the ViewPoint System. These are connected to the instrument and serve as a return path (a "ground") for the energy. During surgery, the instrument alerts the surgeon if the "circuit" isn't complete.
Treatment times average less than 3 minutes, and surgeons report a setup time of less than 2 minutes. Patients usually experience minimal pain following the procedure, and often return to work the same day.
The latest clinical data
Partial results of the Phase III clinical trial have now been tabulated for 401 eyes of 233 patients. The patients in this sample ranged in age from 40 to 74 years and had a mean preoperative manifest refraction spherical equivalent (MRSE) of +1.82, ±0.60D. Mean preoperative cycloplegic refraction spherical equivalent was +1.86, ±0.63D. Data showed:
|
|
|
|
Postoperative UCVA over time for 401 eyes of 233
patients. |
Visual acuity. Twelve months after CK, 56% of the treated eyes were 20/20 or better, and 92% were 20/40 or better. (See chart, right.) Also, 63% were within a half diopter of the intended refraction; 89% were within 1 diopter; and 99% were within 2 diopters of the intended refraction.
Refractive stability. This appears to be achieved after about 6 months. The mean change in MRSE in an early sample of patients from the Phase III trial showed a change of:
- 0.26D between the third and sixth month
- 0.08D between the sixth and ninth month
- 0.11D between the ninth and twelfth month.
The last two amounts of change in refractive error would be considered normal in a patient who had not had surgery.
Safety. In clinical testing:
- No complications or permanent adverse effects have been associated with the surgery.
- No patient lost two or more lines of best-corrected visual acuity (BCVA) after 1 year.
- Induced cylinder was less than or equal to 1.0D in 92.2% of eyes at 12 months, and no eyes developed more than 2D of induced cylinder.
- Endothelial cell counts, measured in the central, mid- and peripheral cornea, showed no statistically or clinically significant changes from baseline over time.
Comparing the options
With several treatments soon to be available for mild hyperopia, it's worth comparing the leading alternatives:
CK vs. LASIK. Clinical results for the two procedures are similar, but CK has several advantages over LASIK:
- CK doesn't ablate any tissue within the visual axis.
- CK avoids flap-related complications and safety issues.
- CK is much easier for the surgeon to perform.
- Because CK requires less equipment and less preparation, it can be performed in your office under a microscope or at a slit lamp. It doesn't require assistance from a technician.
- The ViewPoint System is portable. It's roughly the size of a VCR and weighs less than 15 pounds.
- The ViewPoint System costs much less than a laser.
- CK leaves a larger effective optical zone than LASIK because the diameter of corneal steepening is greater.
- LASIK transects corneal nerves; CK causes minimal damage to nerves.
- Following CK, the worst refractive complications are regression or induced regular astigmatism. LASIK can induce irreversible irregular astigmatism.
LASIK has two chief advantages over CK:
- LASIK can treat a broader range of hyperopic error.
- LASIK patients recover from the surgery faster, and without the minimal discomfort CK patients experience.
CK vs. LTK. LTK (laser thermal keratoplasty) uses a laser to heat the corneal tissue and induce the desired shrinkage. The two approaches have several significant differences:
- LTK's laser generates heat at the corneal surface. This produces a conical-shaped burn that diminishes in proportion to the distance below the surface, resulting in a penetration depth of about 50% and a gradient of tissue temperature. In contrast, the CK probe is inserted into the tissue, generating even, consistent heating that reaches deeper. Several studies have concluded that depth of treatment determines the permanence of the correction.
- To generate a greater refractive correction, LTK increases the energy put into each spot in the cornea. In contrast, CK increases the number of treated spots, not the amount of energy used.
- LTK's effect can be tempered by conditions on the corneal surface. CK's effect isn't.
Comments from the field
Marguerite B. McDonald, M.D., clinical professor of ophthalmology at Tulane University School of Medicine and director of the Southern Vision Institute in New Orleans, is medical monitor for the CK clinical trials and a paid consultant for Refractec.
|
|
|
|
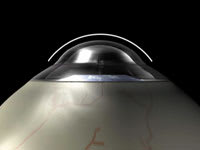
The ViewPoint CK System, from Refractec Inc. |
|
"Hyperopic patients are older than the average myope, and most haven't worn glasses. By the time they pursue surgery, dry eye is a problem. But they expect to heal as fast as their 21-year- old daughter! A flap-free alternative is a great solution.
"Also, the relatively small cost of the CK instrument is an important plus. I think it will offer financial relief to doctors and allow many more surgeons to enter the refractive surgery field."
Peter Hersh, M.D., director of the Cornea and Laser Eye Institute and professor of ophthalmology at the UMDNJ-New Jersey Medical School, comments, "CK is easy, safe, less costly, and probably will be done in an office setting by the patient's own ophthalmologist, without the extra effort or intimidation involved in having LASIK.
"Many of my CK patients see better both at distance and at near. A study we conducted of our patients found that 37 out of 72 treated eyes (51%) had both a distance and near visual acuity better than or equal to 20/40 following CK."
Robert Maloney, M.D., director of the Maloney-Seibel Vision Institute in Los Angeles, also participated in the clinical trials. "My hyperopic LASIK patients sometimes have significant problems with dry eye. Also, they sometimes report haze, blur, ghosts or haloes following LASIK. None of my conductive keratoplasty patients report these problems.
"Overall, my patients love the procedure. We now have a big waiting list of people who don't want LASIK, but want to have CK done as soon as it's approved."
An affordable alternative
The ViewPoint System will cost $48,500, with disposable tips sold at $100 each. Refractec hopes to have approval and reach the marketplace by Spring of 2002.
For more information about CK or the ViewPoint System, visit www.refractec.com on the Internet, call Lauren Kanner at (800) 752-9544, or e-mail info@refractec.com.
Are you aware of new products or technology that have made (or are likely to make) a significant difference in practice? Contact Christopher Kent at kentcx@boucher1.com to find out about possible coverage in a future issue.