Patient
Management
Managing Co-Existing
Cataract and Glaucoma
An update on key areas of decision-making for combined surgeries.
By Leslie Jones, M.D., and L. Jay Katz, M.D., FACS, Philadelphia, PA.
As we weigh whether to perform concurrent surgeries for our patients with cataract and glaucoma, our main goals should be visual improvement and glaucoma stabilization. Advances in technology and continued modifications in surgical technique have lead to remarkable improvements in the success and safety of combined surgery, including faster postoperative recovery, which make these goals attainable.
|
|
|
|
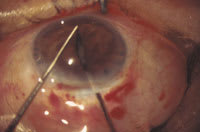
Techniques we're now using to enlarge the pupil, including bimanual stretching, pictured here, have made concurrent cataract and glaucoma surgery safer and easier. |
|
To help bring you up to date, we'll highlight some improvements, offer guidance on patient selection and management and address some of the latest thinking and controversy in this area. We can start with a few improvements that have elevated the safety and success of combined surgery, including:
Cataract incision size. In days past, intracapsular and extracapsular cataract extraction required 10- to 12-mm incisions. Today, with phacoemulsification and foldable IOLs, we can use 3- to 4-mm incisions, which are similar in size to the typical trabeculectomy flap. Not surprisingly, this has improved the success of the glaucoma filtering surgery. Small incision surgery with foldable IOLs has also significantly reduced the risk of intraoperative hemorrhage.
Pupil management. Techniques we're now using to enlarge the pupil, such as sphincterotomies, iris retraction with hooks, and bimanual or instrumental stretching, have made surgery safer and easier. These approaches also allow us to retain smaller, round pupils that are functional and more cosmetically appealing.
IOP control. We've been able to improve intraocular pressure control after combined procedures by employing a number of techniques and adjunctive treatments. For example, a two-site approach using a clear cornea incision for cataract removal can preserve the conjunctiva for filtration sites. In addition, releasable sutures and laser suture lysis allow for slower, and thus safer, reduction of IOP in the weeks following surgery.
Also, it appears that intraoperative application of mitomycin C to limit subconjuctival fibrosis has yielded better long-term control of IOP. Two separate studies have demonstrated a benefit to using intraoperative mitomycin C in combined procedures. Both Carlson and Cohen and their colleagues compared intraocular pressure outcomes in two groups of patients in randomized protocols. One group received intraoperative mytomycin C; the control group did not. With an average follow-up of 12 to 20 months, patients receiving mytomycin C had significantly lower intraocular pressure and required fewer medications to control it than those in the control groups. (See "For More Information".)
|
Possible Challenges and Complications |
||
|
Although the risks associated with cataract surgery in glaucoma patients have been reduced, a number of potential complications and challenges can arise during combined (and sequential) procedures. |
||
| INTRA-OP | POST-OP, EARLY | POST-OP, LATE |
| Big nucleus, small pupil | Wound leak | Loss of pre-existing bleb |
| Zonular/capsular rupture | Choroidal effusion/shallow AC | Loss of bleb |
| Anterior capsule tear | Aqueous misdirection | Central vision "wipe out" |
| Suprachoroidal hemorrhage | Suprachoroidal hemorrhage |
Hypotony maculopathy "Blebitis" endophthalmitis |
Decisions tailored to each patient
Along with these advances, the individualization of patient care is crucial to the success of combined surgery for cataract and glaucoma. To choose our surgical approach, we must assess the overall status of each patient's glaucoma. The stage or severity of the glaucoma, the number and type of glaucoma medications, and the patient's compliance and tolerance of the drugs are essential factors that help formulate the operative strategy.
For example, an eye with severe glaucoma and a very high pressure despite medical therapy is likely best addressed by first performing a glaucoma filtering procedure, then returning to the operating room later to remove the cataract.
In certain eyes with early glaucoma that's controlled with minimal treatment (one or two medications), cataract extraction alone may suffice, because both phacoemulsification and extracapsular cataract extraction techniques have been shown to lower mean intraocular pressure. Ideally, certain medications, i.e., miotics and prostaglandins, should be discontinued at least 1 week preoperatively and for 1 month postoperatively to reduce the potential for inflammation.
Kim DD, Doyle JW, Smith MF. Intraocular pressure reduction following phaocemulsification cataract extraction with posterior chamber lens implantation in glaucoma patients. Ophthalmic Surg Lasers 1999 Jan;30(1):37-40. Bobrow JC. Prospective intrapatient comparison of extracapsular cataract extraction and lens implantation with and without trabeculectomy. Am J Ophthalmol 2000 Mar;129(3):291-6. Carlson DW, Alward WL, Barad JP, Zimmerman MB, Carney BL. A randomized study of mitomycin augmentation in combined phacoemulsification and trabeculectomy. Ophthalmology 1997 Apr;104(4):719-24. Cohen JS, Greff LJ, Novack GD, Wind BE. A placebo-controlled, double-masked evaluation of Mytomycin C in combined glaucoma and cataract procedures. Ophthalmology 1996 Nov;103(11):1934-42. Gianoli F, Schnyder CC, Bovey E, Mermoud A. Combined surgery for cataract and glaucoma: phacoemulsification and deep sclerectomy compared with phacoemulsification and trabeculectomy. J Cataract Refract Surg 1999 Mar;25(3):340-6. Gimbel HV, Penno EE, Ferensowicz M. Combined cataract surgery, intraocular lens implantation, and viscocanalostomy. J Cataract Refract Surg 1999 Oct;25(10):1370-5. |
|
We usually recommend combined surgery for patients who have moderate to advanced glaucoma, borderline or uncontrolled intraocular pressure, and are being treated with two or more glaucoma medications. We often consider performing a trabeculectomy at the time of cataract surgery, even if IOP is medically controlled, to offset the risk of perioperative pressure spikes. So, whether the goal is short-term control of eye pressure postoperatively or long-term stabilization of the intraocular pressure, a combined procedure is preferable.
We must take other factors into account as well. Preoperative evaluation may reveal ocular features that will affect intraoperative decisions regarding cataract removal and enhance the chance of successful glaucoma surgery. For example:
- conjunctival mobility and pre-existing bleb location are determinants of surgical site
- pupil size after dilation determines whether intraoperative pupil stretching will be necessary
- pre-op gonioscopy with attention to peripheral anterior synechiae helps us to ascertain whether an anterior chamber implant or a sutured posterior chamber lens would be preferable in an eye with inadequate capsular support.
Current controversies
Along with all the techniques now available for performing combined procedures comes controversy regarding the best approach. Surgeons disagree on whether a limbal or fornix-based conjunctival flap is best; whether to use one or two sites; and the optimum concentration and duration of mytomycin C. Opinions also vary regarding the construction, shape, and size of the scleral flap and the choice of foldable intraocular lens, i.e., silicone versus acrylic.
Furthermore, recently, proponents of deep sclerectomy and viscocanalostomy have offered reasons for preferring these "non-penetrating" procedures to trabeculectomy in conjunction with phacoemulsification. Gianoli and colleagues have compared the combination of phacoemulsification with deep sclerectomy to standard phacoemulsification with trabeculectomy in a randomized, prospective clinical trial. They've demonstrated similar short-term results in visual and intraocular pressure outcomes.
In a retrospective review, Gimbel and associates have compared a one-site and two-site approach in patients undergoing phacoemulsification with viscocanalostomy. These investigators found that a reduction in intraocular pressure was obtained along with relatively good visual outcomes for a small number of patients with limited follow-up. Further longitudinal, large population comparative studies will hopefully help resolve some of these issues.
Anticipating possible complications
Although the risks associated with cataract surgery in glaucoma patients have been reduced, a number of complications can occur during combined (or sequential) procedures.
Intraoperatively, problems inherent with large nuclei, small pupils, and weak zonular support occur more frequently in eyes with glaucoma, especially those with pseudoexfoliation. Postoperatively, a persistent wound leak and/or hypotony may lead to problems with infection, choroidal effusion and shallow/flat anterior chambers. Delayed suprachoroidal hemorrhage and aqueous misdirection may cause pressure spikes and flat anterior chambers. Even uncomplicated cataract surgery may promote subconjunctival fibrosis and loss of a pre-existing bleb. Hypotony maculopathy may cause vision loss, and the incidence of late endophthalmitis rises in the presence of thin blebs.
Despite these attendant risks, success with cataract surgery in glaucoma patients has increased remarkably over the past decade because of advances in technology and technique. Better guidelines and the best ways to tailor the surgical approach to individuals continue to evolve.
Dr. Jones, who has conducted research in a variety of areas, is currently completing a glaucoma fellowship at Wills Eye Hospital.
Dr. Katz is attending surgeon at the Wills Glaucoma Service and an associate professor at Thomas Jefferson University in Philadelphia.