Tomorrow's Practice-Builder
A look at emerging treatments for presbyopia and designing your
blueprint for success.
BY WARREN D. CROSS, M.D., HOUSTON, TEXAS
Since 1993, I've been actively researching and performing surgeries for the correction of presbyopia. This is an exciting new area for my practice, just as it is for all of ophthalmology. While our myopic, hyperopic, and even astigmatic patients have been enjoying the successes of the latest surgical technologies and techniques, our presbyopes still await a solution designed for them.
But, fueled by some early successes with experimental procedures, our efforts are gaining momentum. The potential here is huge. As the Wall Street Journal reported in March, 90 million Americans over age 40 suffer from presbyopia. I believe that the number of patients who will want presbyopia surgery will result in 2 to 3 times the market penetration that we've seen with LASIK.
At the grassroots level, FDA approval of a procedure specifically for presbyopia will dramatically improve the value of having a balanced practice serving patients of all ages. And practices that are prepared could literally change overnight.
While I believe it's important to ultimately determine which theory correctly explains the cause of presbyopia, I believe it's just as important to seriously consider the merits of all intellectually reasonable approaches to treating it.
With that as our backdrop, let's review the status of current efforts, and consider what we can do now from a practical standpoint to get ready for what will be a new era in vision correction for us and our patients.
Status report
We can divide our current attempts to surgically correct presbyopia into two main categories. The first group merely changes the eyes' focal distance, as in monovision LASIK, or produces multifocal images for the retina to see and evaluate, as with a multifocal intraocular lens (IOL). These approaches attempt to trick the brain into being able to see at near and distance by integrating multiple images. They don't attempt to modify the physiology of the eye.
The second group of procedures does attempt to modify the eye, allowing the lens to "focus" again. These procedures either "pull the eye out," "squeeze the eye in," "increase the rigidity of the eye" or "decrease the rigidity of the eye."
Let's take a more specific look at current and upcoming modalities:
-
Surgical modification of the cornea. As indicated above, these procedures really don't change the ability to accommodate, but the ability to focus at near. The most common is monovision LASIK, which is highly predictable. However, no more than 80% to 85% of patients can tolerate this situation. All patients who are contemplating this treatment should undergo a trial by wearing monovision contact lenses. For any practice, these trials are a time-consuming and expensive use of personnel resources. Furthermore, not all patients can tolerate contact lenses well enough to even evaluate the monovision possibility.
The patients best-suited for monovision are those who are already successful monovision contact lens-wearers. We also must realize that monovision may not provide acceptable functional vision for pilots, those who drive a lot or who are active in sports, especially tennis or baseball. These patients really desire correction of their distance vision plus real ability to accommodate at near.-
Some attempts are being made outside of the United States to use the excimer laser to create a multifocal cornea. Dr. Luis Ruiz in Bogota, Columbia, for example, has compiled some interesting early data, which certainly may help us understand the role of the cornea in vision. But at this point, most surgeons are uncomfortable with the risk of inducing irregular astigmatism, which exists in keratoconus or other conditions, especially after previous refractive surgery.
-
Sunrise Technologies' Laser Thermal Keratoplasty (LTK) is already FDA approved to correct certain levels of farsightedness. It induces myopia without the need for a flap or crossing the visual axis in any way. Those points, along with the fact that it's fast, painless laser surgery, make LTK an appealing procedure for patients. It's appealing for surgeons as well because of its simplicity. Practices can expect to invest approximately $200,000 in the laser.
From a patient management standpoint, overcorrections can result; patients often require enhancements; and irregular drying of the cornea or an eye shifting off-axis during the procedure can produce mild to moderately severe astigmatism. From a technical standpoint, the laser-induced thermal burn is cone shaped, not uniformly cylindrical, and doesn't extend into the corneal stroma at a uniform, constant temperature. The resulting collagen contractions can reverse with time, but nomograms in use outside the United States treat up to 6D of hyperopia, and the effects can last a lifetime in some patients. Results will improve with experience. Sunrise recently received Korean regulatory approval to treat hyperopia and presbyopia. -
Refractec Inc. reported in April that the FDA accepted its filing for pre-market approval of conductive keratoplasty (CK) with the ViewPoint System. CK shares with LTK the advantages of being a fast, painless procedure that doesn't cross the visual axis. Instrumentation is fairly simple and relatively inexpensive, costing about $50,000. The technique is also relatively simple.
The device delivers low voltage, radio frequency energy (350 kHz) when inserted into the peripheral cornea. According to Dr. Marguerite McDonald, of New Orleans, La., "The stability and/or regression after treatment has been comparable to or slightly better than hyperopic LASIK. The reoperative rate appears to be lower than that generally experienced with LTK. Each corneal thermal burn in CK is focused and manually marked and placed. This requires the surgeon to be meticulous in the marking of the cornea, placement of the probe and keeping the probe tip perfectly clean for each application."
Current FDA-approved use covers spherical hyperopia between 0.75D and 3D. Corrections of higher spheres and astigmatism are anticipated in the future. A U.S. clinical trial for the correction of presbyopia has begun.
LTK, and CK when it's approved, have strong appeal for patients who have concerns about the LASIK flap. They're an ideal opportunity for practices to begin marketing to, attracting and treating presbyopic patients.
-
-
Intracorneal lenses. Dr. Richard Lindstrom has reported attempts to implant a small-diameter intracorneal lens to correct presbyopia. The hydrogel lens is designed with a bull's eye in the center for near vision and a periphery for distance vision. It's inserted through a simple lamellar dissection in the cornea. Only 15 patients have been implanted. Results are mixed but promising. The average patient lost about one line of acuity at distance, but improved from J-9 to J-2 at near. Six of the patients said they never use reading glasses. However, in spite of generally good results, four patients requested explantation of their implants. The study is continuing.
-
Incisions at or near the limbus. Another group of procedures, popularized by Dr. Spencer Thornton, involves incisions at or near the limbus or the cornea/sclera. Some incisions are made with a diamond knife and others with a laser handpiece. Because all surgical incisions tend to scar and contract, some surgeons, most notably Dr. Hideharu Fukasaku, propose that implants made of silicone and other materials be sutured into the incisions to preserve the incisional space.
These procedures actually seem to activate accommodation, generally producing approximately 1.50D. -
Laser presbyopia reversal (LAPR). The use of an infrared laser, which incorporates a beam-shaping delivery unit and scanning mechanism, to make incisions at the limbus was patented by SurgiLight Inc. in March. LAPR is similar to many procedures currently performed by most surgeons. The technique involves making eight incisions outside the optical zone in the sclera in a spoke-like pattern. Although LAPR is based on the theory that the lens becomes larger with age, inhibiting accommodation, no one is sure how the procedure improves near vision or why regression doesn't seem to occur.
J.T. Lin, Ph.D., president of SurgiLight, theorizes that the trough remaining after laser excision becomes filled with subconjunctival tissue soon after surgery. He believes that the post-op tissue is more flexible than the original scleral tissue.
Most patients experience a change in accommodation of approximately 1 diopter. But SurgiLight surgeons have reported some postoperative patients with 5D or more of accommodation.
While 1.50D of increased accommodation may work well for activities at arm's length, such as working at a computer, it may not be enough to enable older patients to read. Possible complications include infection, subchoroidal leakage with hypotony and unacceptable cosmetic results.
U.S. clinical trials are expected to begin within a year. -
IOLs. The Array multifocal IOL is marketed and successfully used by many surgeons as a technique for the correction of presbyopia. The optics, particularly in bright light, are good. Plus and minus refractive errors can be corrected at the same time by adjusting the IOL power.
This is obviously an ideal presbyopia modality for cataract surgeons because they're proficient with the techniques and already have the necessary phacoemulsification equipment.
Attention must be paid, of course, to the risks of an intraocular procedure, such as infection, retinal detachment and cystoid macular edema. In addition, proper patient selection is crucial. The lens design produces glare associated with oncoming lights in darkness. This doesn't bother every patient, but the explant rate is significant. Older patients may be accepting, but younger, more demanding patients often are not. This aspect of the multifocal IOL complicates the prediction of outcomes.-
A handful of companies are currently working on accommodating IOLs. The acrylate accommodative lens from HumanOptics is undergoing multicenter studies in Germany. It's set to be introduced into the European market this fall.
-
Also, the Phase II clinical trial of the CrystaLens, a silicone multipiece from C&C Vision, is expected to be completed in 3 or 4 months. According to medical monitor Dr. Stephen Slade, the results currently exceed FDA requirements for the study. One patient, an ophthalmologist who had bilateral implants, has been happy with his postoperative vision. His uncorrected distance and near vision is approximately 20/25. The only problem is that the IOL power is slightly off in one eye (not plano), and he had some slight postoperative astigmatism that he felt prevented him from having perfect vision at distance and near without correction.
Dr. Slade explained that the "mechanism allowing the lens to accommodate begins with the ciliary muscle contracting. With contraction, the ciliary body 'bulks up,' increasing its volume and putting pressure on the vitreous. The peripheral squeezing of the vitreous forces the central vitreous to move forward about 1 mm; 1 mm of anterior movement of the lens produces about 2.50 diopters of accommodation."
So far, contracture of the capsular bag hasn't been a problem. Dr. Slade said that a YAG capsulotomy was recently performed on another patient in whom the lens was working. "No problems have been noticed or reported since the YAG, and we don't expect any," he said. -
On another front, Dr. Georges Baikoff recently reported the results of implanting CIBA Vision's Vivarte multifocal, foldable phakic anterior chamber IOL in six eyes of five patients in Europe, ages 55 or older. Preoperatively, all patients had uncorrected distance visual acuity of 20/20 and J1 near vision with a 2.5D add. Up to 6 months post-op, three eyes had uncorrected distance vision of 20/20 with J1 vision with no add. Another had uncorrected distance acuity of 20/25 and J1 with no add. The IOL was removed from two eyes because of poor sizing, with no adverse effects. The Vivarte is a one-piece that incorporates semiflexible haptics with characteristics of PMMA. The optic has properties similar to those of hydrophilic acrylic polymers.
Implanting accommodating intraocular lenses involves learning essentially nothing new for the average ophthalmologist. The most important aspect of the surgery, other than good cataract technique, is the ability to determine the correct power of the lens. It's paramount that the final refraction be perfect, with little astigmatism.
-
-
Implantation of scleral segments. This is currently the most aggressive approach to inducing accommodation. It involves a combination of scleral tunnels, similar to those we use in cataract, trabeculectomy and some retinal surgeries, and implantation of segments or splints.
The segments are implanted approximately 3 mm posterior to the limbus. In experienced hands, these procedures can result in 2.5D to 7D of increased ability to see at near. (Some of our practice's results appear in the SRP chart ) There is still considerable argument about why and how these implants work. Dr. Ronald Schachar theorizes that they work by increasing the space between the edge of the lens and the ciliary body.
In contrast, Dr. Baikoff, who implants similar-sized implants in a placement similar to Dr. Schachar's, theorizes that accommodation occurs because the sclera is flexed inward, relieving the tension on the lens equator, allowing the lens to focus according to Helmholtz's theory.
PresbyCorp reports that Phase I of the FDA trial of its scleral expansion bands (SEBs) is complete. The data have been sent to the FDA. The company hopes to obtain approval for a significantly larger, Phase II study later this year.
One aspect of SEBs that appeals to patients is that they can be removed at the slit lamp. As far as practice expenses, the PresbyCorp instruments, course and segments currently cost about $25,000. That includes enough segments to perform procedures on 50 eyes. The company is also introducing an automated tunnel maker, which is expected to cost about the same as a LASIK microkeratome.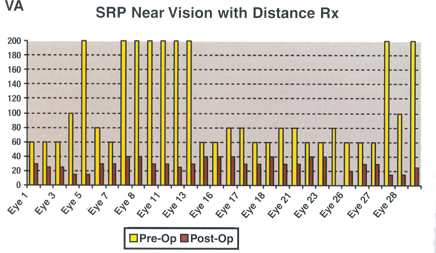
My first group of patients to undergo surgical reversal of presbyopia (SRP) with scleral expansion bands. Data represent 6 months to 2 years follow-up.
Warren Cross, M.D.
Becoming involved
While many of these treatments still await FDA approval, doctors interested in building a presbyopia segment of their practices can begin laying the groundwork now. As I mentioned earlier, such practices should be offering the already-approved treatments for farsightedness.
Pacific Laser Eye Center, a network of more than 600 optometrists in the western United States, is working with Richard Meister, M.D., to create what they hope will be the country's premier presbyopia practice. They currently use the already-FDA-approved LTK procedure as their centerpiece for attracting and treating presbyopic patients. One member of their group, Jon Morrison O.D., was the first optometrist to undergo surgical reversal of presbyopia. Many of the practice-building strategies we discuss in this article are modeled after the efforts being made at Pacific Laser.
Active refractive surgery practices are in the best position to address presbyopia. One of the first things they should do is determine the average age of their LASIK patients. Even practices that have lowered the age of their patient base will find that when they can treat presbyopia with something other than monovision, they'll be able to increase the number of patients they help by 10 or 20%. Others will find that the average age of their LASIK patients is higher than they thought, putting them in an even stronger position. This was the case for us and for Dr. Andrew Caster in Beverly Hills, Calif., who found the average age of his LASIK patients to be 45. Based on that, he believes he'll be able to easily increase his refractive caseload by 30% with the approval of a presbyopia procedure.
Furthermore, many post-LASIK patients make good candidates for presbyopia-specific treatments. They've already shown an interest in elective surgery, have been happy with the results and now want to be able to see at near as well. Among my patients who've undergone implantation of scleral segments, 14 eyes are post-refractive surgery. The first 12 patients of Dr. Meister were all previous LASIK patients. "I've been very pleased with the results these patients have obtained," he said. "The range of accommodation is 2 to 4 diopters, with an average result of 3.6 diopters."
In addition to active refractive surgery practices, those with strong O.D. referral networks have a better chance than others of succeeding with presbyopia, according to practice management consultant Joseph Fitzgerald of JHF and Associates in Laguna Niguel, Calif. Optometrists already have a large number of presbyopes in their practices. That being said, it's also likely that practices that aren't part of large referral networks can succeed by beginning to build interest among their own patients now. However, they may have to spend more on advertising. Practices that generate large percentages of new patients through word-of-mouth referrals also may be able to succeed without a large O.D. referral network.
Regional factors may affect potential success as well. The emerging presbyopia surgeries will be moderately to very expensive for patients, which doesn't bode well for practices in lower-income areas. Colleagues in small, rural practices have been quick to tell me that the availability of such procedures would have little effect on them. Practices in medically conservative areas, such as the Northeast, might find that their patients and colleagues will be much slower to accept the new procedures. Conversely, practices in areas where residents value physical fitness and appearance will experience much higher interest.
Another important aspect of evaluating the potential in a practice's patient base is whether the average age of the residents in the neighborhood is getting higher or lower. Neighborhoods with mostly contact lens patients and their children are not very good starts.
A review of what procedures are performed in the practice, along with reimbursement levels and payers is crucial, too. As we were deciding whether to add presbyopia procedures to our armamentarium, our office schedule was tight, and it seemed impossible to add new procedures. Looking at our patient profiles and payer mix, we decided to opt out of our HMOs. This move has proved to be wise. It significantly increased the resources we have available for presbyopic and other refractive procedures.
Building interest and demand through education
We've found that a hefty amount of those resources needs to be spent on education -- for our surgeons, patients and referring practitioners. This is paramount now in the early stages of our attack on presbyopia. Surgeons and their staff members need to attend meetings where the theories and techniques are being discussed. This will enable them to determine which procedures are appropriate for their patients and familiarize them with possible complications.
It's also necessary to create and familiarize staff members with scripts for answering common questions. The scripts should be provided to referring doctors as well. Providing different answers to the same questions doesn't instill a sense of confidence in already nervous potential surgical patients. (See "Common Patient Questions About Scleral Expansion Bands,")
For our patients, we are currently the best source of information, especially for explanations of the different approaches and theories. To build interest and demand, doctors and staff members in our practice let all patients nearing presbyopia know that we'll be able to treat them with reading glasses, bifocals, monovision LASIK, LTK, or bifocal contact lenses, but that when the time comes, they can also consider a newer surgical procedure like SEBs. We recommend this approach to practices we proctor as well. We tell our presbyopic patients that if they ever get tired of their reading glasses or the other inconveniences of presbyopia, they can set up an appointment, and we'll talk about the surgeries that are possible.
Many patients are eager to talk now, and we've performed several surgeries outside of the United States. Others want to wait for FDA approvals before undergoing a procedure, but do want to be put on our "interested list," which we've been compiling for 3 years.
We're also providing patients with brochures and articles that we've clipped, and we're working on our own CD that will include articles and information about our practice's presbyopia services. Also, our experience strongly suggests that a good Web site regarding presbyopia is necessary. While a site may cost anywhere from $5,000 to $35,000 dollars, and take a great deal of development time, it's an important tool for establishing patient loyalty and our foothold in presbyopia correction.
All of this education takes time, however. And these patients frequently have complicated work schedules, which makes scheduling informational visits difficult. To accommodate them, practices should consider changing their office hours. We have some evening hours and have interested patients come in at the end of the day or during lunch hour.
|
Patient Management |
Each new and emerging procedure for the correction of presbyopia will have new and different patient management challenges. Most, if not all, of the surgeries will require more postoperative "handholding" than LASIK. Corneal tear management will be important. Practices will have to have the necessary medications and supplies, such as punctal plugs, on hand and establish appropriate protocols. The use of thicker artificial tears and lubricating gels at night may be necessary. Scleral implant patients have some specific management requirements. Because the conjunctiva is opened, platelet-inhibiting drugs, most commonly aspirin, need to be stopped. All patients have to be examined the next day to rule out anterior segment ischemia. Intraocular pressures must be checked in case patients have developed iritis. Patients must be informed of the possibility of temporary astigmatism following surgery. This could last 2 to 12 weeks. The current technique involves two, or occasionally more, small sutures to close the conjunctiva. Sometimes the sutures aren't well hidden and therefore cause irritation and patient concern. Many patients experience discomfort for the first 1 to 4 months while reading at near. This must be explained to them, and your staff and co-management team must be supportive. Dr. Barrie Soloway, a PresbyCorp FDA investigator in New York, has demonstrated that post-op exercises are important for maximizing accommodative results. The necessary training and coaching takes time and careful follow-up, and getting patients to comply is difficult. The conjunctiva must be evaluated periodically to be certain that it properly covers the segments. If exposure occurs, the conjunctiva will need to be resutured. In extreme cases of dry corneas that don't respond to maximum treatment, I've found cyclosporine drops to be a great help. This medication is currently available through the Leitners compounding pharmacy, in San Jose, Calif. As I state in the accompanying article, knowing and controlling patient expectations about the new procedures is absolutely necessary. We can't overstate the importance of preventing misrepresentations and unrealistic expectations to avoid disappointment and major medical-legal problems. Remember that controlling expectations may be more difficult with patients who have been referred to our practices by other doctors. -- Warren D. Cross, M.D. |
Who are these patients?
We do that because this group of patients is unique. Their average age is 45 to 60. So, most aren't old enough for cataracts, but they're somewhat difficult refractive surgery patients because of their presbyopia and dry eye problems. However, we've found that they share many of the same characteristics with our LASIK patients, so they feel more comfortable around them than around our cataract patients.
For those who are actually undergoing a presbyopia procedure, we schedule workups on different days than for cataract patients. This separation of the different patient types is much easier on the office staff as well. Uniformity in the workups enables them to work faster, more efficiently and with fewer mistakes.
The patient care coordinator we hired specifically for refractive and presbyopia patients spends most of her time educating patients. We chose her because she's friendly, but also detail-oriented, which allows her to interact effectively with presbyopia patients, who, like other refractive patients, require more information than the average patient and expect perfect care.
The willingness of these patients to undergo surgeries for presbyopia is amazingly high. Today, their age group takes advantage of all types of anti-aging technologies, such as face-lifts, liposuction, Viagra, etc. To them, the possibility of ridding themselves of their bifocals and reading glasses is exciting. Also, they're generally financially secure. Of all the patients we inform that their presbyopia can possibly be reduced, not more than 20% ask about cost. They assume it's expensive. This is in marked contrast to many LASIK patients, who are generally younger and have financial constraints.
|
Scleral Expansion Bands for Glaucoma |
Scleral expansion bands (SEBs) for the correction of presbyopia are also being evaluated to treat primary open-angle glaucoma (POAG). The preliminary results suggest that SEBs have an ability similar to pharmaceuticals to lower intraocular pressure. Dr. Aaron Rifkind suspects that the Canadian POAG study results may look even better than those obtained in the United States. He expects to report on those soon. It's conceivable that with the many and significant complications of our current glaucoma surgical techniques, the SEB glaucoma indication could be FDA-approved before the presbyopia indication. Large glaucoma practices will do well when SEBs are approved because the procedure will warrant insurance coverage. Some data on my patients (27 eyes at 6 to 24 months post-op) are shown at left. -- Warren D. Cross, M.D. |
Setting your pace
Even if a practice has decided that it wants to be involved in presbyopia correction, and its patient base makes it well-suited for success, surgeons still must determine the right level of involvement. I chose early participation in development of the procedures, generating interest among my patients and performing procedures on interested patients outside the country prior to FDA approval. But other surgeons may find this isn't the route for them.
First of all, because this area is rapidly evolving, I strongly feel that the surgeon must be ready to commit to being actively involved in the procedures for at least 5 to 10 years. Otherwise, the necessary investments in equipment, training, inventory, time, and changing the profile of the practice don't make much sense.
Second, one must have a fairly high tolerance of risk to involve more than a few patients in the experimental procedures because possible long-term problems aren't yet known. Also, new techniques and theories surrounding the different procedures are developing every day, so techniques used today may be obsolete or incorrect tomorrow.
Third, not every ophthalmologist believes that presbyopia is correctable, or that it's in the best interests of patients or ophthalmology to correct it. So, if anything goes wrong, one can expect little support from peers. To avoid criticism, every case must be perfect, including flawless perioperative care and informed consent. But because so few cases have been done, all possible complications haven't occurred. To many surgeons, this is too lonely a position to be in.
Surgeons who want to be involved at this early stage must subscribe to the belief that without the efforts of pioneers, important procedures like corneal transplants and phacoemulsification would've never been discovered and perfected.
A win-win for patients and practices
At whatever level practices decide to become involved, with proper preparation, the treatment of presbyopia will be a family of surgeries they can grow with.
Dr. Cross is head of a 4-M.D., 1-O.D. multispecialty clinic with three offices. He specializes in cataract and refractive surgery and presbyopia. He's a founder and the director of Foundation Surgery Affiliates multispecialty surgery centers. He owns a small amount of stock in PresbyCorp, which he purchased himself. The company reimbursed his surgery costs for procedures performed during the development of its scleral expansion bands, but Dr. Cross isn't currently financially involved with the company. He is also one of the investigators for Allergan's alpha cyclosporine for dry eyes.
Can I see at near and distance after surgery? How long will my vision improvements last? What happens if anything goes wrong; can I be fixed? When I have cataract surgery will the segments still work? When I have cataract surgery, will it interfere with the presbyopia surgery? Does the procedure involve a laser? Does it hurt? What is the risk to my vision? How many days will I be off from work? |









