Spotlight
on Technology and Technique
Plasma Capsulotomy
A newly approved technology puts
a whole new spin on this procedure.
BY CHRISTOPHER KENT,
SENIOR ASSOCIATE EDITOR
Most ophthalmologists in the United States are now aware of the Fugo Blade, which uses plasma technology to create incredibly sharp and virtually resistance-free incisions. The unusual characteristics of this blade -- including its ability to effortlessly cut through tissue as thick as cowhide -- are now triggering the development of new surgical techniques.
Because this breakthrough technology has been approved by the FDA for use in capsulotomy (with approval for other procedures anticipated in the years ahead) it's worth taking a look at some of the ways in which a capsulotomy performed using the Fugo Blade differs from previous procedures.
|
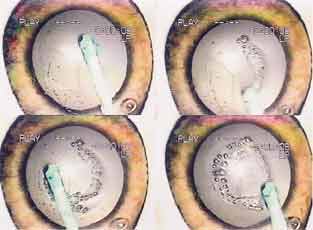
Left: A closeup of the Fugo
Blade tip, showing the plasma energy field coating the cutting filament. |
||
|
|
|
|
How the blade works
The Fugo Blade is a lightweight, handheld, radio-frequency electrosurgical device that generates a cloud of plasma particles around a tiny filament (about as thick as a human hair) at the end of the handpiece. (See image, left.) The plasma particles dissolve the molecular bonds of the material they come in contact with, creating an incision 20 to 40 times sharper than an incision made with a diamond blade.
The plasma blade, which was invented by Richard Fugo, M.D., Ph.D, is the only electrosurgical unit that produces a cutting field that's visible as a microscopic column of light. The unit is portable, and powered by flashlight size, rechargeable batteries. (One charge of the batteries powers the unit for more than an hour.)
|
|
Other Applications |
|
The remarkable cutting ability of the Fugo Blade has prompted researchers to adapt this technology to a number of different applications. Protocols being performed offshore include: Retinal surgery. The Fugo Blade cuts through dense fibro-vascular membranes easily, with no traction on tissue and Glaucoma
surgery. Offshore surgeons are using the blade to place 150-micron filtration tracks in both the pre-iris area and in the pars
plana. (These procedures are performed
transconjunctivally.) A small bleb is raised with
Lidocaine. At the end of the procedure, the bleb is pushed to its natural anatomic location so the conjunctival perforation is at a reasonable distance from the intraocular perforation. Corneal surgery. The blade's energy field can be used to "erase" corneal scarring. This technique is extremely helpful when treating aggressive, recurrent pterygium cases. Other surgeries. Other offshore protocols include: - Surgeons are performing and enlarging capsulotomies in Marfan's patients without dislocating the lens. - In pediatric cataract cases, surgeons are using the Fugo Blade to form strong, reliable anterior capsulotomies that can be repaired and enlarged quickly and safely. - Protocols using the Fugo Blade for ophthalmic plastic surgery and presbyopia reversal surgery are both producing promising results. |
Fugo Blade technique
Here are some key differences between a standard capsulotomy and capsulotomy performed with a Fugo Blade:
- Incising and enlarging the capsule. Because the blade cuts without resistance, tissue isn't torn during the capsulotomy. In fact, using the Fugo Blade may remind you of using a paintbrush on canvas. Gently applanating the anterior capsule with the activated tip makes an immediate, smooth incision into the capsule. (This also makes the capsulotomy go very quickly: On average it takes about 5 seconds.)
To perform capsulotomy, you can use one continuous circular incision or connect several arcuate incisions on the capsule. (Fugo Blade radial incisions don't spontaneously progress.) To enlarge the capsulotomy, make arches along the original capsulotomy rim or radial incisions into the capsulotomy rim (or use a combination of both methods). - No red reflex is required. When using a Fugo Blade, visualizing the procedure isn't a problem. One surgeon who works outside the United States uses the blade in small, out-of-the-way villages to perform cataract surgery, using only loops.
- Use of viscoelastic. It's possible to perform anterior capsulotomies with the Fugo Blade under viscoelastic, air or balanced salt solution. (Novice surgeons should use
viscoelastic.)
When using viscoelastic, you may observe cavitation bubbles during incisions. Employing a viscoelastic such as Occucoat will help to minimize these, but more experienced surgeons will find that the bubbles aren't a serious problem. - Repairing tears. If a tear in the capsule occurs during surgery, simply make an incision with the Fugo Blade perpendicular to the acute tearing edge. The new incision will act as a bulkhead barrier, stopping the spontaneous tearing. (Because you may want to enlarge the incision or repair an inadvertent tear during surgery, it's advisable to leave the handpiece in the sterile field even after the capsulotomy is complete.)
- Cortical coagulum. When working with pathologic cataractous lenses, a thin rim of coagulum may form in the pathologic cortical material under the capsulotomy. You can easily remove the coagulum during phacoemulsification; it won't have any significant impact on the cataract surgery.
Capsulotomy vs. capsulorhexis
Two differences between a capsulorhexis (in which the capsule is torn) and a capsulotomy performed using a Fugo Blade are worth noting:
- A capsulotomy rim made using the Fugo Blade is strong and discreet but has less elasticity than the rim of a capsulorhexis. The tradeoff is that a surgeon can easily increase the size of a capsulotomy using the Fugo Blade.
- During capsulorhexis, mechanical force vectors are directed and focused at an inadvertent tear in the capsulorhexis margin, and they can continue to split the tear through to the posterior pole. (This is sometimes referred to as the "purse string effect.") A tear in a Fugo Blade capsulotomy is much less likely to extend out into posterior pole.
A step toward the future
The Fugo Blade represents a whole new approach to surgery -- and not only for capsulotomy. The increased control it affords will make it possible to expand surgical capabilities, minimize complications, and handle both routine and complicated cases more efficiently and successfully.
Currently, surgeons are required to become certified to use this technology. For more information, contact Dawn Michelle DelCampo, president of Medisurg Research and Management Corporation, at 100 West Fornance Street, Norristown, Pa. 19401, or visit www.fugoblade.com on the Internet.
Ophthalmology Management would like to thank Dr. Richard Fugo for technical assistance with this article.