Cataract Surgery
after Refractive Procedures
Determining corneal power is a challenge.
Here are two ways to improve your outcomes.
By Jack T. Holladay, M.D., M.S.E.E.,
F.A.C.S.
With the increasing popularity of refractive surgery -- especially laser-assisted in situ keratomileusis (LASIK) -- more cataract patients are presenting with surgically reshaped corneas. This can be a problem for the cataract surgeon.
To perform successful surgery, we must determine the health of the cornea, its optical quality (to ensure that the re-duction in vision is caused by the cataract and not the cornea), and its refractive power. The last factor is especially important because corneal power measurement usually determines the accuracy of the outcome. However, corneal power is difficult to measure when dealing with a surgically altered cornea.
Most instruments used for determining central cornea refractive power measure only the anterior corneal surface. To calculate corneal power, keratometers and topographers assume that the posterior cornea is about 84% of the radius of the anterior surface. Unfortunately, this assumption isn't true after refractive surgery on the front surface of the cornea. (See "Standard Net Index of Refraction,")
Also, keratometers measure the paracentral power, not the central power, so another error is introduced. Some instruments, such as Bausch & Lomb's Orbscan II, do provide information about the posterior surface of the cornea, but at this time the information they provide isn't sufficiently accurate to allow precise calculation of corneal power.
These factors lead to inaccurate estimates of corneal power, and those lead to poor outcomes following cataract surgery. However, two other techniques can be used: the calculation method and the hard contact lens trial method. These methods, which are described below, aren't perfect, but they're usually better than direct measurements. (Whatever method you use, following myopic refractive surgery I recommend choosing the flattest reliable value for the corneal power. That will help to minimize a hyperopic outcome.)
Using the calculation method
To use the calculation method to determine central corneal refractive power, you'll need three measurements:
- the patient's K-readings before the refractive surgery
- the refraction before the refractive surgery
- the stabilized refraction following the refractive surgery.
- (Note: The latter measurement should've been taken before any real or apparent myopic shift was caused by nuclear sclerotic cataracts or posterior subcapsular cataracts. To be safe, it shouldn't be taken more than 3 months after the refractive surgery.)
The idea is to subtract the change in refraction at the corneal plane (caused by the keratorefractive procedure) from the K-readings measured before the procedure. This method usually produces excellent results because these numbers are usually accurate to within ±0.25D.
Here's an example of this calculation: Suppose your patient's numbers were as follows:
- Mean preoperative K: 42.50D @ 90° and 41.50D @ 180° = 42.00D (average)
- Preoperative refraction: -10.00 + 1.00 x 90°, Vertex = 14 mm
- Postoperative refraction: -0.25 + 1.00 x 90°, Vertex = 14 mm
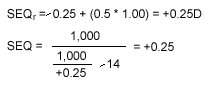
Step 1: Determine the sphero-equivalent refraction at the corneal plane (SEQc). To do this, use the sphero-equivalent refraction at the spectacle plane (SEQs) at a given vertex, where
To determine preoperative and postoperative SEQ at the corneal plane, plug in the appropriate numbers:

Preoperative:

Postoperative:
Step 2: Calculate the change in refraction at the corneal plane by subtracting the postoperative SEQc from the preoperative SEQc:
-8.38 - (+0.25) = -8.63D.
Step 3: Determine the calculated postoperative corneal refractive power by subtracting the change in refraction at the corneal plane from the mean preoperative K:
42.00D - 8.63D = 33.37D.
This gives you the calculated central power of the cornea after the refractive procedure. (If the IOL formula you're using requires two K-readings, simply enter this number twice.)
Using the hard contact lens trial method
|
|
|
|
When working with non-surgically-altered corneas, most IOL calculations use the anterior radius of the cornea and a net index of refraction of 1.3333 to calculate the total corneal power. The latter number is based on average differences between anterior and posterior curvature in normal, unaltered corneas (slightly revised based on actual outcomes). Unfortunately, the relationship between anterior and posterior surfaces is changed by refractive surgery, so this index of refraction is no longer reliable. One exception to this rule is RK patients with optical zones larger than 4 mm. Evidence indicates that RK (unlike LASIK and PRK) causes similar changes in both anterior and posterior radius of curvature, so using the standard net index of refraction number usually produces good outcomes. However, as the optical zone shrinks, accuracy diminishes. -- Jack T. Holladay, M.D., M.S.E.E., F.A.C.S. |
Important note: This method will only work if your patient's cataract allows refraction to within ±0.50D. This usually requires a visual acuity of 20/80 or better.
First, determine the patient's sphero-equivalent refraction using normal methods. Then, take a plano hard contact lens with a known base curve, place it on the patient's eye, and repeat the refraction.
- If the refraction doesn't change with the contact lens in place, the cornea must have the same power as the base curve of the contact lens.
- If the refraction shows a myopic shift with the lens in place, the base curve of the lens is stronger than the cornea by the amount of the shift.
- If the refraction shows a hyperopic shift, the base curve of the lens is weaker than the cornea by the amount of the shift.
For example, suppose your patient has a current sphero-equivalent refraction of +0.25D at the corneal plane. With a plano hard contact lens with a base curve of 35.00D placed on the cornea, you find that the spherical refraction changes to
-2.00D at the corneal plane (a 2.25D myopic shift).
Because the patient had a myopic shift with the contact lens, the cornea must be weaker than the base curve of the contact lens by 2.25D. Therefore the cornea must be 35.00 - 2.25, or 32.75D. (This is slightly flatter than the value obtained using the calculation method, so this is the value I would use.)
In equation form:
- SEQ refraction without hard contact lens = +0.25D
- Base curve of plano hard contact lens = 35.00D
- SEQ refraction with hard contact lens = -2.00D
- Change in refraction = -2.00 - (+0.25) = -2.25D (myopic shift)
Now we add the base curve of the contact lens to the change in refraction to get the mean corneal power: 35.00D + -2.25D = 32.75D.
Making the best of it
As technology progresses, new and improved instrumentation will eventually make it possible to measure accurate corneal refractive power in post-refractive surgery patients without having to resort to these somewhat labor-intensive methods. But for now, these two techniques are the most reliable way to ensure a good outcome -- and a happy patient.
Dr. Holladay subspecializes in refractive surgery and is clinical professor of ophthalmology at Baylor College in Houston. He has invented a number of ophthalmic instruments and programs that are used throughout the world, and has received the Senior Honor Award from the American Academy of Ophthalmology, the Binkhorst Medal from the American Society of Cataract and Refractive Surgery, and the Ridley Medal of Honor from the European Society of Cataract and Refractive Surgery.








