CLINICAL NEWS: MEDICAL AND PRODUCT UPDATES
AGE-RELATED MACULOPATHY
Sunlight exposure
According to researchers in Wisconsin, excessive sunlight exposure early in life may be associated with an increased risk of developing early age-related maculopathy (ARM) in a person's later years.
From 1988 to 1990, researchers performed a baseline examination of 3,684 subjects, ages 43 to 86. Five years later -- from 1993 to 1995 -- researchers questioned the subjects to see how many had developed early ARM.

The 5-year incidence of early ARM was 8.2% overall. (The incidence rate was 9.9% among those aged 43 to 54 years, and 22.6% among those aged 75 to 86.)
Researchers found that subjects who had spent 5 or more hours a day outside during the summer were twice as likely to develop early ARM, compared to those who spent less than 2 hours a day outside. This association remained after researchers made adjustments for:
- alcohol consumption
- cigarette intake
- vitamin use.
Use of hats and sunglasses provided only slight protection. Blondes and redheads were at a slightly greater risk than brunettes.
Lead study author, Karen J. Cruickshanks, M.D., pointed out that the study's population consisted of subjects living in the predominantly non-Hispanic, white town of Beaver Dam, Wis. Dr. Cruickshanks noted the findings may not be applicable to all populations. Nonetheless, she says, "Early ARM may be partly preventable through modification of lifestyle factors."
Arch. Ophthalmol. 2001; 119: 246-250.
GLAUCOMA
Latanoprost
Latanoprost (Xalatan) may cause migraine headaches, according to Bonnie Weston, M.D., at the University of South Alabama.
Dr. Weston reported on three patients who experienced headaches after taking latanoprost.
Two of the cases involved men in their sixties. Over-the-counter analgesics failed to relieve their headaches. But once both patients stopped using latanoprost, their headaches disappeared. One patient was still headache-free after 4 months of follow-up, and the other patient was headache-free after 1 year of follow-up.
The third case involved a 54-year-old woman with primary open-angle glaucoma who had been prescribed latanoprost nightly for her left eye. The night after her first dose, she developed a severe headache, which wasn't relieved by acetaminophen or codeine phosphate. The next day, she didn't have the headache; however, the headache recurred for 3 more nights after taking latanoprost. The headache didn't recur on the fourth night, and the patient has continued taking latanoprost with no more headaches.
Dr. Weston suggests that you discontinue latanoprost if a patient develops headaches.
Arch. Ophthalmol. 2001; 119: 300-301.
AMD AND PATHOLOGIC MYOPIA
New Visudyne results
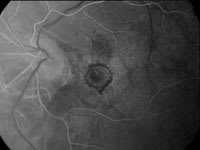
Novartis Ophthalmics has announced the results of two clinical trials on the effectiveness of Visudyne therapy. Both studies were multicenter phase IIIb randomized, placebo-controlled studies.
The first study showed that Visudyne therapy benefits wet age-related macular degeneration (AMD) patients with occult choroidal neovascularization (CNV). The second study showed that Visudyne reduces the risk of vision loss in patients with CNV due to pathologic myopia.
|
|
|
|
Clinical results show that Visudyne benefits two types of patients. |
In the first study, 339 AMD patients enrolled at 28 centers throughout North America and Europe. After 24 months, 46% of the enrollment population treated with Visudyne lost less than three lines of vision on a standard eye chart, compared to 33% of the placebo group. The difference of 13% between the treated group and the placebo group is statistically significant and higher than the 4% difference seen after 12 months of Visudyne treatment.
In the second study, investigators treated 120 patients with CNV due to pathologic myopia. After 12 months, 86% of the patients treated with Visudyne lost less than three lines of vision on a standard eye chart, compared to 67% of the placebo group (a difference of 19%). After 24 months, the difference dropped from 19% to 7%, still in favor of Visudyne. However, 40% of the Visudyne-treated patients gained one or more lines of vision versus 13% of the placebo group.
In both studies, patients treated with Visudyne received, on average, five treatments over 24 months. Investigators found no new safety concerns.
GLAUCOMA
Lumigan vs. timolol
Allergan has released 6-month data from two ongoing phase III trials of its glaucoma drug, bimatoprost ophthalmic solution, 0.03% (Lumigan). The data indicate that Lumigan is clinically superior to timolol 0.5% in lowering intraocular pressure (IOP) over a 24-hour period. (Allergan presented the data at the American Glaucoma Society meeting.)
Lumigan is part of a new class of drugs called synthetic prostamides. Prostamides exist naturally in ocular tissue, and are believed to lower IOP.
Allergan's double-masked phase III trials involved 1,198 patients with glaucoma or ocular hypertension. Allergan randomized the patients into three different treatment groups. The first group received Lumigan once a day; the second group received Lumigan twice a day; and the third group received timolol twice a day.
Pooled data from the two trials indicated that patients receiving Lumigan once a day achieved significantly greater IOP reductions from baseline levels than patients receiving timolol twice a day. (Lumigan once a day also was more effective than Lumigan twice a day.)
Allergan's results demonstrated that the IOP-lowering effect of once-a-day Lumigan was sustained throughout the duration of the study. The mean IOP in the Lumigan once-a-day group was at least 2 mm Hg lower than that in the timolol group.
According to an Allergan spokesperson, "Lumigan is safe and well tolerated by patients." Reported adverse events occurring in approximately 15% or more of patients were conjunctival hyperemia and eyelash growth.
On March 16, the FDA approved Allergan's drug application for Lumigan to treat glaucoma.
MACULAR DEGENERATION
Gene finding
Scientists have isolated another gene that plays a role in macular degeneration. The gene is an elongation of very long-chain fatty acids (ELOVL4). The scientists found ELOVL4 at high levels in the retina.
A spokesperson for the scientists, Kang Zhang, M.D., said, "If you damage this gene really badly, you'll get adolescent-onset, severe macular degeneration at a young age -- Stargardt's disease. But if you damage it to a lesser extent, it will predispose you much more than the general population to age-related macular degeneration (AMD)."
This isn't the first macular degeneration gene that researchers have identified. Another gene, ABCR, is thought to play a role in both AMD and Stargardt's disease, and other genes have been linked to juvenile-onset macular degeneration.
"We're on track," says Dr. Zhang, "to hopefully isolate all the genes for macular degeneration within the next 5 years. I think it will then take another 5 years to develop drugs to intervene in the process."
Nature Genetics 2001; 27: 89-93.
CATARACTS
Anterior capsular contraction
According to Japanese researchers, after cataract surgery, the anterior capsular opening shows greater contraction among diabetics, especially those with diabetic retinopathy, than among nondiabetic patients.
Study author Satoshi Kato, M.D., says, "Anterior capsule contraction is a complication after cataract surgery. Anterior capsular contraction (and opacification) interferes with postoperative funduscopy of the peripheral retina, retinal photocoagulation and vitreous surgery."
Dr. Kato and his colleagues measured the area of the anterior capsular opening after cataract surgery in 31 eyes of 31 diabetic patients and 30 eyes of 30 normal controls. Measurements were taken 3, 6 and 12 months after surgery.
Each time Dr. Kato's group measured the anterior capsular opening, it was significantly smaller in diabetics, compared to patients in the control group. Patients with diabetic retinopathy also had significantly smaller anterior capsular openings than patients without diabetic retinopathy.
Also, Dr. Kato found that the percent reduction of the anterior capsular opening was significantly associated with the presence of diabetes and aqueous flare intensity 1 year after surgery.
Dr. Kato says, "We must be diligent when performing cataract surgery, and make sure the complication of anterior capsular contraction doesn't occur."
Br. J. Ophthalmol. 2001; 85: 21-23.